Drug Interactions
There are thousands of prescription drugs, with more and more new medications introduced every year, and hundreds of dietary supplements and herbal products available in pharmacies and stores in the U.S. Consumers should be aware of the dangers of combining certain drugs and other substances, including supplements, herbal products, foods, and beverages.

Patients who take prescription medicine should know that in addition to potential side effects, it’s important to be aware of how the drugs interact with other drugs, supplements, and certain foods and beverages.
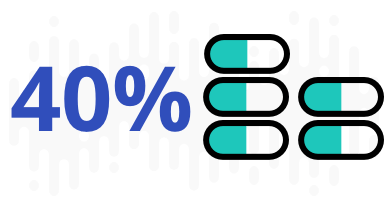
According to the government’s National Health Survey, after adjusting for age, about 34 percent of adults are taking 1 to 4 prescription drugs, and 11 percent are taking 5 or more.

Multiple Medications and Supplements
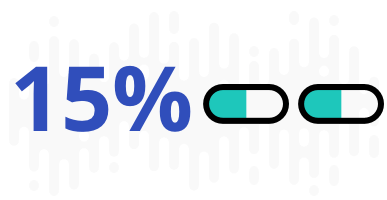
A 2016 study in JAMA Internal Medicine found that older adults are increasingly using multiple medications and supplements. The study found 36 percent regularly using five or more drugs or supplements and 15 percent at risk for potential major drug interactions.
Particularly dangerous reactions can occur when a person takes two or more drugs that have similar properties that magnify each other’s effects. Also dangerous is a situation in which the person ingests drugs with opposite properties that cancel the benefit of both drugs. Another common adverse interaction can occur when one drug alters the concentration of another drug.
Interaction Risks
Not all drugs interact with each other. However, the more medications a patient takes, the more likely it is that some medications will interact with each other. With proper oversight from a doctor, it can still be possible to take multiple medications safely and avoid interactions.
The drug-interaction risks are:
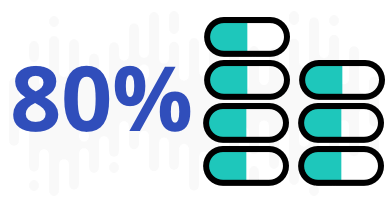
This is a particular concern for older people, as close to half take five or more medications, and 12 percent take 10 or more.
Risks Vary
For people in hospitals, adverse drug interactions may be the fourth leading cause of death.
Interactions can affect how medications work in the body. They can enhance or decrease the effects of the drugs. They can also contribute to the possibility of dangerous side effects. The results of an interaction vary depending on the person and other things like the particular drugs that are interacting, the doses, the timing and even genetics.
In some instances, drug interactions discovered after medication approval were so dangerous that the drugs were pulled from the market.

Drug Interaction Health Risks
Possible side effects from interactions also vary widely.
- Drowsiness
- Rapid heartbeat
- Changes in blood pressure
- Bleeding
- Flushing
- Diarrhea
- Ruptured Achilles tendon
- Coma
- Death
Interaction Factors
Drug interactions are complicated and largely hard to predict. Not everyone who takes drugs that are known to interact with each other will experience the effects.
- Genetics
- Age
- Lifestyle, such as the patient’s diet and her exercise habits
- Other medical conditions
- The length of time both drugs are taken
It’s best to talk to your doctor or pharmacist about the potential effects of combining medications, as well as dietary supplements and even certain foods and beverages.
Drug Interaction Types
- Drug-drug interactions
- Drug-drug interactions happen when drugs react with each other. One example of this is when a patient takes a sedative to fall asleep and also has allergies and takes an antihistamine. Combining both of those drugs can make the patient even sleepier, slow their reactions and make it dangerous to drive or operate machinery.
- Drug-food/beverage interactions
- Drug-food/beverage interactions happen when drugs interact with what you eat or drink. Alcohol is a well-known example of this. Drinking an alcoholic beverage while taking some medications that make you sleepy can additionally slow your reactions and make you sleepier. Taking some drugs that affect blood pressure or heart function might interact with coffee or other beverages containing caffeine.
- Drug-condition interactions
- Drug-condition interactions happen when you have a medical condition that reacts with certain drugs. Nasal decongestants may constrict blood vessels even further in patients with high blood pressure, for example. And if you are allergic to certain substances, you may not be able to take some drugs. For example, patients with gluten may not be able to take some drugs that include gluten as a filler. This is also true for patients with decreased kidney or liver function, which may reduce the amount of drug that gets removed by these organs. Lastly, some genetic conditions may affect how fast drugs are metabolized, which might increase or decrease the drug’s effects.
- Drug-supplement interactions
- Drug-supplement interactions are when your medication reacts to herbal or dietary supplements. These interactions could have effects similar to drug-drug interactions.

Drug-Drug Interactions
A drug-drug interaction typically involves what’s known as a precipitant drug and an object drug. The object drug is the one with a therapeutic affect that is changed by the drug interaction. The precipitant drug is the one that affects the pharmacologic action of the object drug.
Common precipitant drugs — drugs that influence the action of other drugs — include nonsteroidal anti-inflammatory drugs and certain antibiotics. Common object drugs include warfarin, fluoroquinolone antibiotics, antiepileptic drugs and oral contraceptives.
Some drugs act both as object drugs and precipitants.
The consequences of drug interactions are as diverse as the possible drug combinations. Nonsteroidal anti-inflammatory drugs taken at the same time as corticosteroids, anticoagulants or antiplatelets can increase the risk of gastrointestinal bleeding. Fluoroquinolones taken at the same time as corticosteroids can lead to increased risk of rupture of the Achilles tendon.
Some common drugs and examples of how they interact with other drugs, supplements and food:
Antidepressants
The most widely prescribed class of antidepressants today is selective serotonin reuptake inhibitors (SSRIs). They work to elevate the serotonin levels in the brain, which is thought to ease the symptoms of depression.
One serious complication, serotonin syndrome, can occur when an SSRI interacts with other drugs that have similar effects, especially pain medications and other drugs for psychiatric illness. The onset of serotonin syndrome can occur within minutes and can be deadly if not treated immediately.
St. John’s wort, a dietary supplement used to treat depression, can cause serotonin syndrome when it is combined with an SSRI. SSRIs also are known to interact with over-the-counter antihistamines, causing extreme drowsiness.
Common SSRIs include:



There are no proven interactions with food when a patient takes an SSRI. At least one study, however, suggests that eating kiwifruit, which has high natural levels of serotonin, can increase the effects of SSRIs on serotonin levels. Also, certain SSRIs can cause an upset stomach or heartburn if they are taken on an empty stomach.
Blood Pressure Medication
Blood pressure-lowering medications include alpha blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta blockers, calcium channel blockers, and diuretics. Approximately 33 percent of U.S. adults either have high blood pressure or take blood pressure-lowering drugs. Blood pressure medications generally should not be taken with OTC decongestants such as pseudoephedrine, because decongestants may increase blood pressure. Also, because caffeine may increase blood pressure, some patients who take blood pressure-lowering medications may need to limit their consumption of caffeine-containing beverages such as coffee.
Diuretics such as hydrochlorothiazide (HCTZ) are commonly used to lower blood pressure. They work by helping the body remove excess water, but this could also affect electrolytes. Diuretics should not be taken with heart-rhythm medications because the combination can lower potassium levels to the point that fatal cardiac arrhythmia can occur.
One food interaction has been documented for HCTZ. Glycyrrhizin — found in black licorice, some sweeteners and herbal teas — can have a negative effect on potassium levels, which can damage the heart.
Proton Pump Inhibitors
Taking proton pump inhibitors, which reduce gastric acid, along with antibiotics can increase the risk of irregular heartbeat, which can be life threatening. A 2016 study found that taking the heartburn drug Prevacid (lansoprazole) at the same time as ceftriaxone, an antibiotic, can make it more likely that the patient will develop a dangerous, life-threatening condition called long QT syndrome, which can be fatal.
When proton pump inhibitors are taken with antibiotics, there is a risk of Clostridium difficile infection, a bacterium with symptoms from diarrhea to colon inflammation that can be life threatening.
Statins
Statins are a class of drugs that reduce cholesterol levels. Within this class, some statins pose a higher risk of drug interactions than others. Fluvastatin, pitavastatin, pravastatin, and rosuvastatin are less likely to have drug interactions than some other statins.
Drugs that can interact dangerously with different statins include gemfibrozil, cyclosporine, clarithromycin, azole antifungals, protease inhibitors and colchicine. Drinking alcohol while taking statins can increase the risk of liver damage.
Muscle and Kidney Damage
One of the most common side effects of statins is muscle soreness. Mixing statins with certain drugs, dietary supplements or foods can damage muscles and even lead to kidney failure. For this reason, patients are advised not to mix statins with prescription oral fungal (yeast infection) medication or vitamin B complex.
Warfarin
Warfarin, a blood thinner, interacts with a number of other drugs and supplements. Some other medications increase the body’s metabolism of warfarin and the risk of thrombosis, or the formation of blood clots.
- Phenytoin
- Carbamazepine
- Rifampin
- Cholestyramine
- Phenobarbital
On the opposite end of the spectrum, some drugs decrease the metabolism of warfarin, which increases the risk of bleeding.
- Fluoroquinolone antibiotics
- Trimethoprim/sulfamethoxazole, which are antibiotics
- Macrolide antibiotics
- Heartburn drugs such as Prevacid (lansoprazole), Prilosec (omeprazole) and Zantac (ranitidine)
Other common drugs that interact with warfarin include simvastatin, acetaminophen, prednisone and omeprazole. Some supplements also interact with warfarin, sometimes increasing the risk of bleeding. These include omega-3 fatty acids, garlic, gingko and saw palmetto.
Leafy green vegetables and other vegetables high in vitamin K can affect warfarin’s ability to prevent clots. Cranberry juice and other cranberry products can also affect how warfarin works.

Food-Drug Interactions
Certain foods can have an effect on the medication you take. This can prevent a drug from working the way it should, increase or decrease a side effect of the drug or cause a new side effect. Medicine can also affect how your body digests and processes food.
Some examples of different food and beverages and how they can affect certain drugs:
Alcohol
According to the National Institutes of Health (NIH), about 71 percent of adults in the United States drink alcohol. Alcoholic beverages can interact with a wide range of medications, including many that are commonly prescribed, and you should consult with your doctor or pharmacist about whether you can drink while taking your prescription drugs.
According to NIH research, 42 percent of adults who drink also use medications that are known to interact with alcohol. This is true for nearly 78 percent of people over 65.
For example, alcohol can add to side effects of some drugs. It can add to the drowsiness caused by antihistamines and it can cause liver damage if you take acetaminophen or other pain relievers and fever reducing medicines. The chance for severe liver damage increases if you drink three or more alcoholic drinks a day. Alcohol can also increase the chances of dangerous side effects with narcotic medications. These risks include coma and death.
Statins and Nitrates
Avoid alcohol if you are taking statins because it increases the chance of liver damage. Drinking alcohol while taking nitrates, which are given for angina (chest pain), may add to the nitrate’s blood-vessel-relaxing effect and dangerously lower blood pressure.
Refrain from drinking alcohol if you’re using theophylline, which is given for asthma. The two taken together can increase the chance of nausea, vomiting, headache and irritability.
Antibacterial and Psychiatric Drugs
Drinking alcohol while taking the antibacterial metronidazole or up to a day after finishing the medication can cause nausea, stomach cramps, vomiting, flushing and headaches.
The antifungal griseofulvin can make the effects of alcohol worse. Together, they can cause a fast heartbeat and flushing.
Alcohol can also add to the side effects, like drowsiness, of certain psychiatric medications, including antipsychotics, antidepressants and sleep medications.
Caffeine
Ingesting caffeine when using bronchodilators can increase the chance of side effects such as excitability, nervousness and rapid heartbeat. Because caffeine may increase blood pressure, it may also reduce the effects of blood pressure-lowering medications.
Grapefruit Juice
Grapefruit juice contains compounds known as furanocoumarins, which change the effects of some drugs. These compounds are not present in other citrus juices. Consequently, grapefruit juice can affect how the body metabolizes drugs, changing the level of the medication in the blood.
- Antihistamines
- Blood pressure medications
- Thyroid replacement drugs
- Birth control
- Antacids
- Dextromethorphan (cough suppressant)
If you drink more than a quart of grapefruit juice a day, it can increase the levels of certain statins, but not all statins, in your body and raise the chance of side effects.
Leafy Green Vegetables
Leafy green vegetables are high in vitamin K and can lower the ability of warfarin to prevent clots. Warfarin works by blocking clotting factors that are dependent on vitamin K.
Foods high in vitamin K include broccoli, cabbage, collard greens, spinach, kale, turnip greens, and Brussels sprouts.
Leafy vegetables also are high in potassium, as are bananas, oranges and salt substitutes. Taking ACE inhibitor drugs and certain diuretics can increase the amount of potassium in your body. Too much potassium can harm you, leading to irregular heartbeat and rapid heartbeats, also known as palpitations.

Drug-Supplement Interactions
On average, Americans spend more than $28 billion each year on dietary supplements. In 2021, people in the U.S. spent nearly $50 billion on dietary supplements. These include vitamins, minerals, herbal and other substances that are purchased over the counter at drug stores, grocery stores and health nutrition stores.
According to a survey of people aged 50 and over by the American Association of Retired Persons, 59 percent of respondents had used supplements the previous month, and 52 percent took them almost daily.
A study published in JAMA in 2016, found that older adults are using more and more supplements. Researchers found an increase of almost 50 percent in the use of multiple supplements, despite, the author wrote, “no evidence of any clinical benefits.”
Some of these supplements can change how the body absorbs, metabolizes or excretes drugs and they may have an effect on how potent the drug is. But research on herb-drug interactions has not been rigorous, and information is mostly inferred from sources such as animal studies and other indirect means.
Still, experts have compiled information about some common supplements and their effect on different prescription medications. Here are a few examples:
Calcium
Calcium supplements may reduce the effectiveness of some drugs, including antibiotics, such as fluoroquinolones and tetracyclines, calcium channel blockers, osteoporosis drugs and thyroid drugs. Calcium may increase the risk of kidney damage by increasing calcium blood levels when taken with antihypertensives including thiazide diuretics and it may increase the effects of digoxin.
Fish Oil
Taking fish oil may reduce the effectiveness of some cancer drugs and may increase the effects of blood pressure medications and blood thinners.
Garlic
Garlic is sometimes taken in the belief that it can treat high cholesterol, heart disease and high blood pressure. The high doses of garlic contained in supplements can act as a blood thinner. This can be dangerous when taking blood-thinning medications and may increase the risk of excessive bleeding. There is some evidence that garlic may affect the body’s metabolism of the HIV antiviral drug saquinavir, but that risk appears to be low.
Taking garlic in supplement form may also reduce the effectiveness of birth control pills, HIV/AIDS drugs, cyclosporine and isoniazid for tuberculosis.
Ginkgo Biloba
This herbal supplement can also thin the blood. Taking it with other substances that have that effect, such as aspirin, vitamin E and warfarin, may increase the risk for internal bleeding or stroke. Ginkgo and ginseng can also have dangerous interactions with certain psychiatric medications, including those given for anxiety. It can reduce the effectiveness of drugs including anticonvulsants, diabetes drugs and HIF/AIDS drugs.
St. John’s Wort
This herbal supplement can make certain drugs less effective. These drugs include medications for HIV/AIDS, heart disease, depression, organ transplants and birth control.
If you are taking digoxin, avoid combining it with St. John’s wort, which may decrease the amount and action of digoxin in your body.

How to Avoid Drug Interactions
When you get a new prescription, you should ask your doctor or pharmacist some questions:
- Can I take it with other drugs and supplements?
- Should I avoid certain food or drinks?
- What signs of possible interactions should I be aware of?
- How does the drug work in my body?
- Where can I get more information about this drug or my condition?
Drug Labels
You should also make sure your doctor and pharmacist know about vitamins and supplements you take, and read the information provided by the pharmacy with your prescription. Carefully read the drug interaction precaution information.
It’s best if you can obtain all your prescriptions from a single pharmacy, which can keep track of all your medications and flag possible interaction issues.
Medication List
It is extremely important to keep a complete list of all your medications and bring that list to every medical appointment to help your doctor check for possible drug interactions. It’s probably wise to carry the list with you at all times. In addition to the name of the medication, you should include the size of the dose (in milligrams, milliliters, or other measurement) and how often you take the drug. You should also ask your doctor and your pharmacist whether there is a chance of drug interactions.
Online Tools
The U.S. Food and Drug Administration has a tool you can find here to help you create a record to keep track of your medicines and dietary supplements.
The AARP also has an interaction checker where you can enter the name of a drug or pick from a list of common drugs and it will give you possible interactions to be alert for.
Avoiding Interactions
Your doctor or pharmacist can take steps to address possible drug interactions.
- Avoiding certain drug combinations because they are too risky.
- Adjusting the dose of one or both of the interacting drugs.
- Spacing the times between taking drugs that interact with each other. For example, certain object drugs may need to be taken at least two hours before or four hours after the precipitant drug, allowing the object drug to be absorbed by the body before the precipitant drug is introduced.
- Monitoring for side effects through laboratory tests or close observation, adjusting dosages as necessary.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

