Reverse Shoulder Replacement Risks, Complications and Device Concerns
Reverse shoulder replacement is a common procedure for patients with rotator cuff damage, but some implants have been recalled or linked to serious complications that required additional surgery. Some people filed lawsuits after their device failed and injured them.
- Last update: June 27, 2025
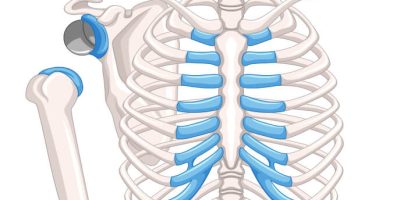
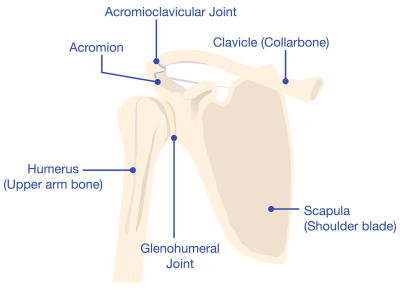
A reverse shoulder replacement is a surgical procedure that uses artificial implants, such as a ball and socket, to mimic the shoulder joint.
A standard shoulder replacement attaches an artificial socket to the shoulder blade and an artificial ball to the top part of the arm bone, which more closely mimics the natural shoulder joint. In a reverse shoulder replacement, the ball attaches to the shoulder blade, and the socket is at the top of the arm bone.
- Reverse shoulder replacements help alleviate chronic pain in people with rotator cuff tears.
- Manufacturers have recalled some devices, which may fail early.
- Early device failure led people to file lawsuits.
Doctors use a reverse shoulder replacement for specific injuries, such as a torn or malfunctioning rotator cuff. People may also be candidates for reverse shoulder replacement if they have had a previous shoulder replacement that wasn’t successful.
While this surgery can help people with chronic shoulder pain, reports of poor design and early failure led some people to file reverse shoulder replacement lawsuits against implant makers. The U.S. Food and Drug Administration (FDA) also informed the public about recalls for early device failure and the potential for additional surgeries.
Common Risks and Complications After Surgery
Potential risks and complications following a reverse shoulder replacement surgery include infections and blood loss, similar to any joint replacement. However, reverse shoulder replacements also have additional, unique complications. For example, dislocation is a common complication with reverse shoulder replacement.
- Anesthesia complications
- Blood vessel injuries
- Dislocations or joint instability
- Fractures of the shoulder bone
- Infections
- Nerve damage
- Reduced range of motion and decreased shoulder strength
According to a study from the journal Clinics in Shoulder and Elbow, complications occur in anywhere between 15% and 24% of reverse shoulder replacements.
Some pain or numbness after the procedure is normal, but patients who experience swelling, bleeding, fever or chills should speak to their doctor right away.
Signs Your Reverse Shoulder Implant May Have Failed
Some post-surgery symptoms — such as persistent pain, swelling, difficulty using your arm or muscle weakness — could mean the implant has failed.
In addition to these physical symptoms, there may be grinding or other noises from the implant.
FDA Recalls and Safety Concerns About Reverse Shoulder Devices
The FDA issued its most serious Class I recall for the Zimmer Biomet Comprehensive Reverse Shoulder System Humeral Tray in 2017. The FDA issues Class I recalls for products that may cause serious injury or death.
Zimmer Biomet recalled the device because of design defects leading to a higher-than-normal rate of fractures and the potential for revision surgery.
In January 2024, the FDA issued a Safety Communication for the Exactech Equinoxe Shoulder System for defective packaging. The defective bags were missing barrier layers that protect the device from exposure to oxygen, potentially causing the device to wear down and fail early.
What to Do if Your Reverse Shoulder Implant Failed
If you suspect your reverse shoulder system may have failed, talk to your doctor right away. They will evaluate your shoulder implant using physical examinations, X-rays and other diagnostic exams as needed to confirm device failure.
If your device has failed, your doctor will discuss your options, which may include physical therapy, medication or revision surgery to replace the failed implant.
What Is Revision Reverse Shoulder Replacement?
Revision reverse shoulder replacement is a complex procedure intended to replace a problematic reverse shoulder implant. It may not be as effective as the initial shoulder surgery, but revision can help improve pain and function after a device failure.
A literature review published in Orthopaedics & Traumatology: Surgery & Research suggested a success rate of about 90% in revision surgery. But the study authors also noted it may take several procedures to reach this success rate.
Some people who needed revision surgery after an implant failed have filed lawsuits against device manufacturers.
Steps to Take if You’re Considering Legal Action
If you are considering taking legal action against a reverse shoulder replacement manufacturer, keep all surgical and medical records. This includes hospital notes and details about the implant model.
These medical records will be important evidence that an attorney can use to see if you qualify for a claim and prove your case in court. If you can’t find all of your records, an attorney may be able to help you locate them.
When you’re ready to hire an attorney, make sure they have experience filing complex medical device injury claims. Take action right away because you have a time limit (called the statute of limitations) to file your claim, and it varies by state.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.