Blood Thinners
Blood thinners limit coagulation, which prevents blood clots from forming. These medications include anticoagulants and antiplatelets. While blood thinners don't actually thin or change the viscosity of blood, their ability to prevent clotting can help protect people from strokes and heart attacks.

What Are Blood Thinners?
Blood thinners are drugs that decrease the risk of a blood clot forming. While the common term “blood thinner” is a bit of a misnomer for these medications, as the thickness of blood itself is not changed, these medications offer important protections to people at risk of blood clots.
Cardiologists and other health care professionals typically prescribe blood thinners for people who have an irregular heartbeat, heart disease, blood vessel disease or deep vein thrombosis (DVT). People who have a history of heart attack or stroke are also often prescribed blood thinners.
- Aspirin
- Brilinta (ticagrelor)
- Coumadin (warfarin)
- Effient (prasugrel)
- Eliquis (apixaban)
- Plavix (clopidogrel)
- Pradaxa (dabigatran)
- Savaysa (edoxaban)
- Xarelto (rivaroxaban)
Excessive and internal bleeding are serious potential risks, resulting in complications from mild bruising to life-threatening hemorrhagic stroke, a type of bleeding in the brain that requires immediate emergency care. Talk to your doctor about possible risks and take medications exactly as prescribed.
Direct oral anticoagulants, or DOACs, have been found to be safer than warfarin for patients with atrial fibrillation. A new study published in November 2022 in Annals of Internal Medicine found apibaxan to be the safest blood thinner among DOACs, including dabigatran, edoxaban and rivaroxaban. Apibaxan was associated with the lowest risk of gastrointestinal bleeding.
How Do Blood Thinners Work?
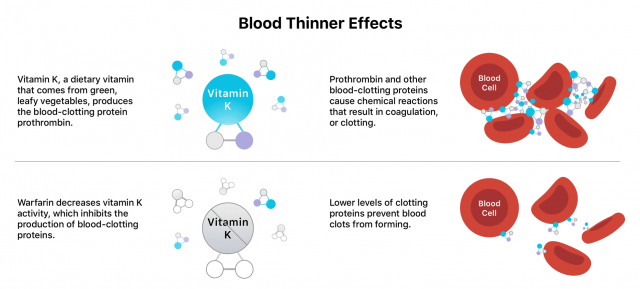
Blood thinners work in different ways. Some block or weaken vitamin K and its blood clotting effects. Others block proteins or enzymes that bind blood cells and platelets. Another type of blood thinner also works to keep platelets from sticking together or to blood vessel walls.
As noted previously, blood thinners don’t “thin” blood. Additionally, they don’t dissolve or break up existing clots. However, they can help prevent existing clots from getting larger.
Types of Blood Thinners
There are a variety of old and new blood thinners, and they fall into one of two categories: anticoagulants, such as warfarin, and antiplatelet medications, such as aspirin. Each impacts the process of blood clotting, called coagulation, in different ways.

Anticoagulants target clotting factors and disrupt them, slowing the body’s process of making clots. Antiplatelet drugs keep platelets from clumping together, preventing a clot from forming.
Anticoagulants
There are several anticoagulants on the market. Warfarin was introduced in the 1950s and remains a popular medication despite the addition of newer blood thinners. The U.S. Food and Drug Administration estimates that approximately 2 million people still take warfarin.
- Coumadin (warfarin): The oldest blood thinner, Coumadin blocks the formation of vitamin K-dependent clotting factors. Its antidote is vitamin K.
- Eliquis (apixaban): An oral medication, Eliquis impacts the production of the enzyme thrombin, which causes blood clotting.
- Heparin: This fast-acting liquid medication is administered via injection. It prevents an enzyme called thrombin from triggering the production of a protein called fibrin that helps the body form clots.
- Lovenox (enoxaparin): This injectable blood thinner is made from heparin but produces a more predictable anticoagulant response than heparin.
- Pradaxa (dabigatran): Taken orally, Pradaxa inhibits the clotting effects of the enzyme thrombin. The FDA also approved Pradaxa oral pellets for children, a first for a blood thinner.
- Xarelto (rivaroxaban) and Savaysa (edoxaban): Xarelto and Savaysa both block a vitamin K-dependent protein called Xa. People who have mechanical heart valves or valvular atrial fibrillation cannot take Savaysa. People who are pregnant should not take Xarelto.
The FDA has approved a handful of blood thinners since 2010, including Pradaxa, Xarelto, Eliquis and Savaysa. The latest addition to the list could be asundexian, which received a fast-track designation from the FDA for more testing in the treatment of irregular heartbeat, heart attack and a specific stroke condition.
Antiplatelet Drugs
The most widely taken antiplatelet medication is aspirin. Doctors often recommend over-the-counter aspirin at varying doses for people at risk of blood clots, heart attacks and strokes.
Though aspirin is available both as an OTC medication and in prescription strength, the prescription medication is typically only prescribed for symptoms of rheumatoid arthritis and lupus. It is sometimes advised to take OTC aspirin in combination with other antiplatelet drugs for people who have acute coronary syndrome or unstable chest pains (angina).
- Aspirin: People at higher risk of a heart attack or stroke often take aspirin. People experiencing symptoms of a heart attack are often advised to take low-dose chewable aspirin and call 911 immediately.
- Brilinta (ticagrelor): This medication is typically prescribed for people who have already had a heart attack. It’s sometimes taken in combination with aspirin.
- Effient (prasugrel): Almost identical to Plavix, the effects of this medication are irreversible.
- Persantine (dipyridamole): It stimulates the production of a group of fatty acids collectively called prostacyclin, blocking platelet activation.
- Plavix (clopidogrel): This antiplatelet drug limits the ability of platelets to clump together. Like Effient, Plavix’s effects are irreversible.
Doctors rarely prescribe antiplatelet drugs to people who already have blood clots. They instead use them as a preventative medication for those with a higher risk of developing clots.
Natural Blood Thinners
Natural blood thinners are nonmedication sources that slow or prevent clotting, but they’re not a substitute for prescription anticoagulants or antiplatelets. They can include ingredients such as alcohol and foods or herbs like garlic, ginger, celery seed and anise seed. Speak with your doctor before adding any natural blood thinners to your daily regimen.
While supplements and homeopathic medicines may be labeled “natural,” they can still potentially have serious side effects or cause an allergic reaction. Many supplement products are unregulated. Taking these substances while also taking prescription blood thinners can increase your risk of bleeding.
When Are Blood Thinners Prescribed?
Doctors prescribe blood thinners for people deemed to have a higher risk of having a heart attack or stroke or developing blood clots. Your doctor may prescribe a blood thinner if you have any of the following conditions or if these experiences apply to you:
- Atrial fibrillation (AFib)
- Blood vessel disease, such as deep vein thrombosis (DVT) or pulmonary embolism (PE)
- Congenital heart defects
- Heart disease
- Heart valve replacement surgery
- After surgery, when blood clots are a concern
AFib is a particular concern because of its high risk factors. Rapid heartbeat or heart palpitations characterize this type of irregular heartbeat. People diagnosed with AFib are five times more likely than people without AFib to have a stroke. And people with AFib who have a stroke are more likely to experience a permanent disability.
DVT and PE are types of venous thromboembolism (VTE), which occurs because of a blood clot in a vein. PE occurs when there’s a blood clot in one of the pulmonary arteries of the lungs, which typically happens when the clot moves from another location such as the legs or arms.
What to Limit When Taking Blood Thinners
Some foods, herbs, spices and oils that have high amounts of vitamin E, salicylates, natural antibiotics or omega-3 fatty acids have natural blood-thinning properties. Consuming them while taking blood-thinning medication can increase the risk of bleeding.
Because some blood thinners block vitamin K, which is involved in coagulation, eating foods that are high in vitamin K can impact how your blood thinner works, especially warfarin. Limit alcohol consumption, drugs and herbal supplements that can counteract warfarin and other blood thinners.
- Alcohol: Light to moderate alcohol use can increase bleeding risks while taking blood thinners, but heavy alcohol use can increase the risk of blood clots.
- Amiodarone: Data is still limited, but this drug used to treat life-threatening heart rhythm issues may cause excess bleeding if taken with blood thinners.
- Antibiotics: A number of antibiotics have varying degrees of risk for interfering with the effectiveness of blood thinners such as warfarin.
- Antifungal Medications: These drugs, including ketoconazole or itraconazole, can increase the effects of blood thinners, risking excess internal bleeding.
- Carbamazepine: Taking this anti-epileptic medication can make blood thinners like warfarin less effective.
- Coenzyme Q10: Evidence is mixed, but some studies show taking CoQ10 makes Coumadin and Plavix less effective.
- Garlic: Garlic is a natural blood thinner and may increase the risk of dangerous bleeding when mixed with an anticoagulant medication.
- Ginkgo Biloba: This herbal supplement also has blood-thinning properties.
- NSAIDs: Nonsteroidal anti-inflammatory drugs affect platelets and clotting. Speak with your doctor before taking medications such as Advil, Aleve, Motrin, Nuprin and Alka-Seltzer.
- St. John’s Wort: This herbal supplement can decrease the effectiveness of many medications, including blood thinners.
- Thyroid Medications: Under certain conditions, thyroid drugs can increase blood thinners’ effects. But changes in thyroid activity also impact anticoagulation factors.
- Vitamin E: Oils including sunflower, wheat germ, safflower and soybean, peanut butter, almonds, red bell peppers, pumpkin and other vitamin-E rich foods can increase bleeding risks when taken with blood thinners.
- Vitamin K: Green leafy foods, including spinach, kale, Swiss chard, parsley, endive, cabbage and asparagus, are high in vitamin K. Also avoid vitamin K supplements.
- Yeast: More study is needed to determine if red yeast rice can increase bleeding risks for people who take Coumadin, Plavix or aspirin.
Discuss your diet and all medications you take with your doctor. If you need to take another medication, such as an antibiotic, discuss the safest options with your physician.
Trimethoprim/sulfamethoxazole (TMP/SMX), ciprofloxacin, clarithromycin, metronidazole, fluconazole, levofloxacin and azithromycin all have a high risk of interfering with the effectiveness of blood thinners such as warfarin. Clindamycin and cephalexin can also interfere with blood thinners, but the risk is considered significantly lower.
Blood Thinner Side Effects
The most common side effects from taking a blood thinner are bruising and the development of a rash. The most serious side effect is uncontrolled bleeding, especially internal bleeding. Hemorrhaging is life-threatening and requires immediate medical attention.
Call 911 or visit urgent care if you cut yourself and can’t stop the bleeding. People who take blood thinners often report excessive bleeding from minor lacerations, cuts and nosebleeds.
- Bleeding more than normal during menstruation.
- Coughing up blood.
- Cuts that won’t stop bleeding.
- Nosebleeds or bleeding gums that won’t stop.
- Severe headaches or stomach pains that won’t go away.
- Stools turning red, dark brown or black.
- Urine turning dark red or dark brown.
Blood thinners can also increase bruising and cause the formation of blood blisters. They may also make you feel weak, faint, dizzy or nauseous. Some side effects specific to antiplatelet drugs include aspirin-induced asthma and the development of nasal polyps.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

