Pradaxa
Pradaxa is a prescription blood thinner. People use Pradaxa to lower the chance of stroke and blood clots. The U.S. Food and Drug Administration warns that suddenly stopping Pradaxa or missing doses may increase the risk of blood clots or stroke. This can cause permanent disability and death. Pradaxa can also cause drug interactions if taken at the same time as certain medications. Side effects of Pradaxa include serious and sometimes fatal bleeding. The FDA gave full approval to a Pradaxa bleeding antidote in April 2018. Boehringer Ingelheim makes Pradaxa. The company recalled a batch of Pradaxa in 2012, citing a potential packaging defect.
- Medically reviewed by Kenneth S. Fill, Pharm.D., MBA
- Last update: March 7, 2025
Pradaxa (dabigatran) is a medication that prevents clots from forming. Because of this, many people refer to it as a blood thinner. Pradaxa can treat and prevent blood clots, which can reduce the risk of stroke.
Boehringer Ingelheim makes Pradaxa. The U.S. Food and Drug Administration first approved Pradaxa in 2010.
What Is Pradaxa Used For?
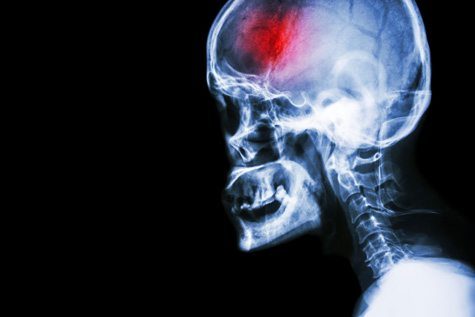
Pradaxa is used in patients with atrial fibrillation (irregular heartbeat) not caused by a heart valve problem. It lowers the risk of stroke in these patients. It does this by lowering the chance that a blood clot will form and move to the brain, causing a disruption in blood flow in the brain.
The FDA also approved Pradaxa to treat deep vein thrombosis and pulmonary embolism in patients who have been treated with injectable blood thinner for five to 10 days.
Deep venous thrombosis, or DVT, is a serious condition that occurs when a blood clot forms in the deep veins in the body, also known as the extremities. This is usually in the legs and thighs. A pulmonary embolism, or PE, occurs when a blood clot becomes lodged in a blood vessel in the lung.
Doctors also prescribe Pradaxa to prevent DVT and PE in patients who have had hip replacement surgery.
How Does Pradaxa Work?
Pradaxa is known as a direct thrombin inhibitor. It blocks the blood’s central clotting agent, thrombin. This lowers the chance of blood clots forming.
Pradaxa Dosage
Pradaxa comes in 75 mg, 110 mg and 150 mg capsules. Most people take 150 mg capsules twice a day.
People with kidney problems may take lower doses of Pradaxa because the drug is eliminated through the kidneys. The FDA advises doctors to check a patient’s kidney function before prescribing Pradaxa and to reassess kidney function throughout treatment with the drug.
How to Take Pradaxa
A patient’s doctor will explain the best way to take Pradaxa. But the drug’s manufacturer instructs patients to swallow Pradaxa whole with a full glass of water.
It advises patients not to break, chew or empty the capsules. Patients can take Pradaxa with or without food.
Pradaxa Overdose
It is possible to overdose on Pradaxa. Overdosing on Pradaxa increases a patient’s risk of bleeding.
If a person suspects a Pradaxa overdose, he or she should immediately contact a poison control center or seek emergency treatment.
Pradaxa Recall
In November 2012, Boehringer Ingelheim announced a nationwide voluntary recall of a single manufacturing lot of Pradaxa 75 mg capsules. The company cited a potential packaging defect.
It warned that a damaged bottle could allow moisture to get into the bottle. This could harm the quality of the drug.
Pradaxa Side Effects
The most serious Pradaxa side effect is uncontrolled bleeding. For five years after the FDA approved Pradaxa, there was no way to reverse these bleeding events, which did lead to death in some patients. There is now an antidote for Pradaxa bleeding, called Praxbind.
Some people have filed Pradaxa lawsuits against Boehringer Ingelheim over bleeding injuries and deaths.
Researchers also have reported incidents of acute kidney failure, stroke and suspected liver failure with Pradaxa use. Other side effects of Pradaxa include gastrointestinal issues like indigestion, upset stomach, burning and stomach pain.
Pradaxa Warnings and Precautions
According to the drug’s prescribing information, you should not take Pradaxa if you have a mechanical prosthetic heart valve.
Pradaxa is also not appropriate for patients with active pathological bleeding or a history of hypersensitivity reaction to Pradaxa.
The FDA requires a black box warning — the agency’s strongest warning — to alert the public of the risk of spinal and epidural hematomas in patients treated with Pradaxa who are receiving neuraxial anesthesia or undergoing spinal puncture.
Pradaxa patients who have medicine injected into their spinal and epidural area, or have a spinal puncture, have a risk of forming a blood clot that can cause long-term or permanent paralysis.
Stopping Pradaxa
Patients should not stop taking Pradaxa without first talking with their doctor. The FDA warns that missing doses may increase the risk of blood clots or stroke. Suddenly stopping Pradaxa also increases the risk of thrombotic events such as strokes.
Pradaxa, Xarelto and Warfarin
People may compare Pradaxa to other blood thinners like Xarelto and Warfarin. The FDA approved the drugs at different times and different manufacturers make them.
| CATEGORY | PRADAXA | XARELTO | WARFARIN |
|---|---|---|---|
| Manufacturer | Boehringer Ingelheim | Bayer and Janssen Pharmaceuticals (Johnson & Johnson) | Bristol-Myers Squibb |
| FDA Approval Date | 2010 | 2011 | 1954 |
| Cost | Almost $6,000 a year | Almost $6,000 a year | $200 a year |
| Uses | Atrial fibrillation not caused by heart valve problem; lowering chances of blood clot forming in heart; deep vein thrombosis; pulmonary embolism | Same as Pradaxa | Same as Xarelto and Pradaxa; plus to reduce the risk of death from heart attacks and other thromboembolic events after a heart attack |
| Bleeding Antidote | Praxbind (2015) | AndrexXa (2018) | Vitamin K |
| Routine Blood Tests Required | No | No | Yes |
Pradaxa Interactions
Patients should let their doctor know about any medications or supplements they take prior to starting Pradaxa. Taking Pradaxa at the same time as certain other medications can lead to drug interactions. Pradaxa drug interactions can not only make the medications less effective, but can also lead to dangerous additive side effects such as excessive bleeding.
- Antacids
- Aspirin and aspirin-like drugs
- Cobicistat
- Cyclosporine
- Dronedarone
- Ketoconazole
- Mifepristone
- Nonsteroidal anti-inflammatory drugs such as ibuprofen naproxen and celecoxib
- Rifampin
- St. John’s wort
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


