Benicar
Benicar is a prescription blood pressure medication manufactured by Japanese drugmaker Daiichi Sankyo. Its active ingredient is olmesartan medoxomil, which is available as a generic formulation. The medication belongs to the angiotensin II receptor blocker, or ARB, drug class and works by blocking a hormone called angiotensin II, which causes blood vessel constriction and high blood pressure.
- Medically reviewed by Amanda Gerberich, Pharm.D. BCPS
- Last update: June 12, 2025
The U.S. Food and Drug Administration first approved brand name Benicar in 2002 to treat high blood pressure. Then in 2003, it approved Benicar HCT — a drug that contains both olmesartan with hydrochlorothiazide, a blood pressure drug from the thiazide diuretic drug class.
In clinical trials, one 20 mg dose of olmesartan reduced blood pressure by about 10/6 mmHg and 40 mg reduced it by about 12/7 mmHg.
Millions of Americans use Benicar and its generics each year.
Olmesartan medoxomil is one of the top 300 most prescribed drugs in the United States in 2017 with over 2 million prescriptions, according to the U.S. Department of Health and Human Services’ most recent Medical Expenditure Panel Survey data.
The combination of olmesartan medoxomil and hydrochlorothiazide was also in the top 300 most prescribed drugs in 2017 with over 1 million prescriptions.
What Does Benicar Treat?
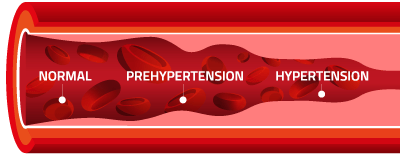
Benicar is indicated for the treatment of hypertension, also known as high blood pressure. It is used to lower blood pressure.
Blood pressure rises as blood vessels constrict. While it’s normal for blood pressure to rise and fall throughout the day, health problems can develop for individuals whose blood pressure remains high for a longer period of time.
Blood pressure is measured by two numbers. The first number, referred to as systolic, represents pressure when the heart beats and is the higher number. The second number, referred to as diastolic, is the pressure when the heart rests in between beats. The blood pressure value is expressed as systolic over diastolic. For example, a systolic of 120 and diastolic of 80 is written as “120/80 mmHg”. A normal blood pressure is less than 120/80 mmHg.
When left unchecked, elevated blood pressure levels greatly increase a person’s risk for heart disease and stroke, leading causes of death in the United States. High blood pressure usually has no accompanying symptoms, so many people are unaware that there’s even a problem.
The Centers for Disease Control and Prevention estimated that 75 million adults have high blood pressure in the United States. It affects approximately one in every three adults.
Just over one half of individuals with high blood pressure are controlled. Seven in 10 of those adults with high blood pressure are taking a blood pressure medication. These individuals are sometimes prescribed a medication such as Benicar or a medication containing the ingredient olmesartan.
For patients suffering from high blood pressure, taking a medication for control, such as Benicar, can reduce the risk of heart attack and stroke.
Who Should Not Use Benicar?
Benicar can result in complications for fetuses, especially in the second and third trimesters, and some of these complications can be fatal to the fetus. Also, the drug should not be utilized in children under one, as it can negatively affect growth and development of the kidneys. Other individuals can experience adverse reactions when taking Benicar.
Benicar is not recommended for the following people:
- Pregnant women
- Nursing mothers
- Children under one year of age
- Patients with blood volume or salt depletion (a lower starting dose should be utilized)
- Patients with stiffening of renal arteries (also called renal artery stenosis)
Benicar Side Effects
The most common Benicar side effect is dizziness. Serious and less common side effects include facial edema (known as angioedema), high potassium levels (also known as hyperkalemia), low blood pressure (known as hypotension), and decreased kidney function.
Also, in 2013, the FDA released a safety announcement warning the public that Benicar has the potential to cause intestinal problems known as sprue-like enteropathy. Symptoms of drug-induced sprue-like enteropathy include severe, chronic diarrhea and substantial weight loss within months to years after beginning use of the medication.
Benicar can also result in fetal toxicity and is not recommended for women who are pregnant. Benicar should be discontinued as soon as possible when pregnancy is detected.
- Back pain
- Bronchitis
- Increase of creatinine phosphokinase (CPK)
- Diarrhea
- Headache
- Blood in urine
- High blood sugar
- Elevated triglyceride levels (fat in the blood)
- Flu-like symptoms
- Inflammation of pharynx or back of throat
- Inflammation of mucous membrane inside the nose
- Sinusitis
- Chest pain
- Fast heart rate
- Peripheral edema
- Weakness/lack of energy
- Vertigo
- Abdominal pain
- Indigestion
- Diarrhea
- Nausea
- High levels of cholesterol in blood
- High concentration of fats in blood
- Excess levels of uric acid in blood
- Decreases in hemoglobin and hematocrit level
- Elevations of liver enzymes and/or serum bilirubin levels
- Increased blood creatinine levels
- Joint pain
- Arthritis
- Muscle pain
- Rhabdomyolysis (a condition causing destruction of skeletal muscle)
- Rash
- Acute kidney failure
- Hair loss
Black Box Warning – Fetal Toxicity
A black box warning appears on a prescription drug’s label when the FDA wants to call attention to serious or life-threatening risks associated with its use. Benicar (olmesartan medoxomil) contains one of these warnings for fetal toxicity. The label says Benicar should be discontinued as soon as possible after pregnancy is detected. This is because olmesartan acts directly on the renin angiotensin system (a system in the body that regulates blood pressure), which can cause injury and death to the developing fetus.
The label says the risks are greater during the second and third trimesters. The risks include reduction of fetal renal function and increase in fetal and neonatal death.
This could lead to a decrease in amniotic fluid and result in fetal lung underdevelopment and skeletal deformations.
Potential neonatal adverse effects include:
- Skull underdevelopment
- Failure of kidneys to produce urine
- Low blood pressure
- Kidney failure
- Death
Benicar Dosages
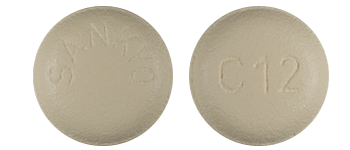
Benicar comes in tablet form in three different prescription strengths: 5 milligrams (yellow/round pill), 20 milligrams (white/round pill), 40 milligrams (white/oval). This drug can be taken with or without food, and it can also be administered with a diuretic and/or other antihypertensive medications.

Dosage Information for Adults
- Recommended starting dosage of 20 milligrams once daily
- If further blood pressure reduction is required after two weeks of taking Benicar, the provider may increase the dose to 40 milligrams.
- Doses above 40 milligrams have not been shown to have any greater effect in patients.
- Twice-daily dosages do not appear to offer any advantage over the same total dose taken once daily.
Dosage Information for Children
- Dosing must be individualized
- Recommended starting dosage in children 6 years of age and older and weighing 44 to 77 pounds is 10 milligrams once daily
- If further reduction in blood pressure is required after two weeks of taking Benicar, the provider may increase the dose to a maximum of 20 milligrams once daily for those weighing under 77 pounds
- If further reduction in blood pressure is required after two weeks of taking Benicar, the provider may increase the dose to a maximum of 40 milligrams for those weighing over 77 pounds
- For children who cannot swallow pills, Benicar may be taken as a suspension.
Drug Interactions with Benicar
It is possible for Benicar to cause adverse reactions when taken concurrently with certain drugs (both prescription and nonprescription). These adverse reactions may include unfavorable side effects and/or decreased effectiveness of Benicar or the other drugs.
- Aliskiren (Brand Name – Tekturna):
- It is recommended that Benicar is not given in conjunction with aliskiren (antihypertensive drug) in patients with diabetes.
- NonSteroidal Antiinflammatory Drugs (NSAID) including Selective COX-2 inhibitors:
- Taking Benicar with NSAIDs, a type of pain medication including ibuprofen (Motrin) or naproxen (Aleve), can lead to decreased kidney function. Taking NSAIDs can also decrease the effects of Benicar.
- Dual Blockade of the Renin-Angiotensin System (RAS):
- Taking Benicar with other ARBs, ACE (angiotensin-converting enzyme) inhibitors (such as Captopril, Ramipril, Lisinopril, Quinapril and others) or aliskiren is associated with increased risks of low blood pressure, high potassium and changes in kidney function.
- Colesevelam Hydrochloride (Brand Name – Welchol):
- Taking colesevelam hydrochloride with Benicar reduces the effectiveness of Benicar. It is recommended that olmesartan is taken at least four hours prior to taking a dose of colesevelam hydrochloride in order to decrease the effect of the drugs’ interaction.
Mayo Clinic Study Confirms Olmesartan-Induced Enteropathy
Twenty-two patients who were seen at the Mayo Clinic between August 2008 and August 2011 were described in a study examining the link between olmesartan and unexplained sprue-like enteropathy. Olmesartan is an active ingredient in Benicar.
To be included in the study, patients had to have chronic diarrhea (lasting more than four weeks) while taking olmesartan. The cause of the symptoms could not be explained by another disorder, such as celiac disease; and finally, discontinuing the drug resulted in clinical improvement.
Mayo Clinic’s 2012 Report
In 2012, Mayo Clinic researchers published this study as a case series of sprue-like enteropathy associated with patients’ use of olmesartan.
2012 Results:
- The 22 subjects involved in the series presented similar clinical results to individuals of 23 adverse event reports identified by the FDA through its FDA’s Adverse Event Report System (FAERS).
- Of the 22 patients from 17 states treated by the Mayo Clinic between the years of 2008 to 2011, 14 required hospitalization with weight losses averaging almost 40 pounds, and one patient losing a total of about 125 pounds.
- None of the patients responded to gluten free diets (used for celiac disease sufferers).
- They were all taking daily doses of olmesartan ranging from 10 to 40 mg.
- When olmesartan was discontinued, the patients’ symptoms improved and they all experienced some degree of weight gain.
Mayo Clinic’s 2013 Report
In May 2013, an article was published describing patients with negative blood tests for celiac disease and villous atrophy, a condition in which the wall of the intestine erodes away.
2013 Results:
- The article reported that some patients without definitive causes for villous atrophy were categorized as having unclassified sprue.
- It was later discovered that some of these patients had villous atrophy associated with their use of olmesartan.
Olmesartan-induced enteropathy was further investigated using prescription refill information and Medicare insurance claims, which showed that patients using olmesartan had a higher rate of being diagnosed with celiac disease than users of other ARBs.
One 2022 clinical study noted the potential of olmesartan medoxomil nanoparticles delivered intranasally to improve the drug’s effectiveness. The engineered bioparticles showed a significant decrease in blood pressure and heart rate, suggesting the potential application of intranasal olmesartan medoxomil nanoparticles.
FDA-Initiated Label Change for Sprue-like Enteropathy
In 2013, the FDA issued a safety announcement about the potential for occurrences of sprue-like enteropathy. This decision came following its evaluation of FAERS, the Mayo Clinic case series and information from the Center for Medicare and Medicaid Services (CMS) database. The FDA also ordered the drug manufacturer to change its labeling on the blood pressure medication to include a warning about this.
In premarketing clinical trials, the incidence of adverse effects reported by Daiichi Sankyo related to olmesartan was similar to those of placebo, and the only negative effect linked directly to olmesartan with greater frequency than the placebo, as reported in the prescribing information, was dizziness. While millions of individuals have been prescribed olmesartan over the last several years, reports of severe gastrointestinal reactions associated with its use are claimed to not have surfaced until later in 2012.
Less than a year after the FDA ordered the label change for Benicar and other drugs containing olmesartan, patients who had suffered sprue-like enteropathy began filing Benicar lawsuits. Daiichi Sankyo, Benicar’s manufacturer, agreed in August 2017 to settle Benicar claims from about 2,300 plaintiffs in cases for $300 million.
In 2006, the U.S. Department of Health & Human Services (DOH) submitted a warning letter to Sankyo Pharma Inc. through its Division of Drug Marketing, Advertising and Communications (DDMAC). The letter requested that Sankyo immediately cease its promotion of certain sales and marketing materials that contained unsubstantiated effectiveness and superiority claims, and omitted or minimalized information on the risks associated with the use of Benicar.
Warning Letter to Benicar Manufacturer
In 2006, the U.S. Department of Health & Human Services (DOH) submitted a warning letter to Sankyo Pharma Inc. through its Division of Drug Marketing, Advertising and Communications (DDMAC). The letter requested that Sankyo immediately cease its promotion of certain sales and marketing materials that contained unsubstantiated effectiveness and superiority claims, and omitted or minimalized information on the risks associated with the use of Benicar.
The omitted or minimalized risk information included:
- Serious pregnancy-related risks
- Renal artery stenosis (narrowing of arteries that carry blood to one or both of the kidneys) precautions
- Risk information regarding the use of Benicar HCT in patients with impaired liver function or systemic lupus erythematosus (the most common form of lupus characterized by extreme fatigue and joint pain)
- Lithium interactions
In addition to the marketing warnings, Daiichi Sankyo faced kickback allegations. The U.S. Justice Department accused Daiichi Sankyo of paying doctors to prescribe Benicar. Daiichi Sankyo paid $39 million to settle the criminal case.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

