Knee Replacement
Knee replacement can help relieve pain from joint trauma or degenerative diseases like osteoarthritis. More than 600,000 people in the U.S. undergo a partial or total knee operation each year, and that number is expected to grow to 3.48 million by 2030.
- Medically reviewed by Jessica D. Hess, Ph.D.
- Last update: March 13, 2025
Knee replacements are surgical substitutions of a knee joint where the femur and tibia bone meet, with an artificial joint or implant. Although the procedure might seem like a modern one, it actually dates back to the mid-1800s.
Medical device companies refined all manner of artificial joints over the past three decades as doctors discovered more demand for them. An increased number of younger (and more active) potential recipients are wearing down or injuring their joints and asking for permanent or semipermanent medical solutions.
- Arthritis
- Osteoarthritis
- Rheumatoid arthritis
- Developmental abnormalities
- Avascular necrosis (bone death)
- Obesity
- Emergency traumas
- Repeated injuries
Doctors recommend knee replacement surgery when patients endure constant pain or when daily life is affected by poor mobility. More than 90% of knee replacement patients experience a significant reduction in knee pain, according to the American Academy of Orthopaedic Surgeons.
Recipients can have a partial knee replacement or a total knee replacement. The difference depends on the recipient’s condition and pain level.

Rising Number of Knee Replacement Surgeries
When medications, therapies and other treatments don’t work, surgery is the next step to reclaiming mobility. A total knee replacement can get a patient back to work or back to a better quality of life.
The number of knee replacement surgeries continues to grow in the U.S. and is projected to reach 3.5 million procedures each year by 2030. This significant increase can be attributed in large part to the growing number of baby boomers (those born between 1946 and 1964) reaching retirement age — when the chance of a worn-out joint is higher — and a rise in obesity and an increased need for follow-up procedures (revision surgery).
Most patients who undergo total knee replacement are between the ages of 50 and 80, but recommendations for these procedures are based on a patient’s pain and disability, not age.
As the number of knee replacements increased, so have the number of problems reported with knee implants. In July 2022, researchers reported on a clinical study that followed a group of adults aged 45 to 74 for five years after they received a total knee replacement. The authors noted excessive sedentary behavior in 91% of the cohort, and inadequate physical activity at five years was apparent for 59% of participants. Additionally, 47% of patients experienced clinically significant fatigue after five years.
Manufacturers have issued nearly 1,000 knee replacement recalls since 2003. But not all defective implants were included in those recalls.
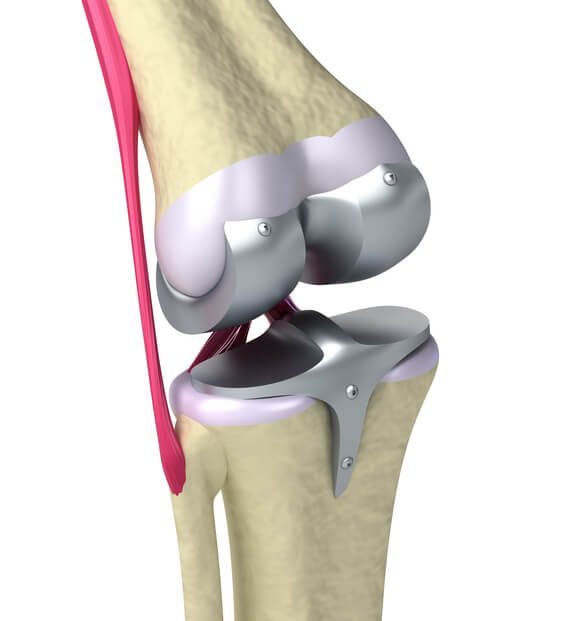
How Do Artificial Knee Joints Work?
The knee joint forms where the femur (thighbone) meets the tibia (shinbone) and fibula (runs alongside the tibia). The patella (kneecap), located on the front of the knee, moves up and down against the femur. These bones are connected by ligaments, muscles and cartilage that help form the joint hinge and give the joint its flexibility.
Although there are four bones around the knee joint, only the femur, tibia and patella are affected by an implant.
While many device companies design and manufacture knee implants, which in turn can be made from a variety of metals, plastics and ceramics, artificial knee joints consist of three components.
- Femoral component
- This metal piece attaches to the end of the femur. It has a groove that allows the patellar component to slide up and down smoothly as the knee bends and straightens.
- Tibial component
- This flat, two-piece metal and polyethylene (plastic) part is attached to the tibia. The metal part sits on top of the tibia and has a stem that is inserted into the tibia for stability. The plastic part, or tibial spacer, acts as a cushion between the metal tibial component and the metal femoral component.
- Patellar component
- This plastic piece is dome-shaped to match the resurfaced shape of the patella. Because the patella rests against the femur, the alignment of the patellar component and femoral component is crucial for proper function. The patella is held in place by the quadriceps tendon and patellar tendon.
These three components are usually cemented in place, but some doctors use a cementless technique that helps the bone grow into the implant to help increase stability.
A cementless technique may be used on patients who are young, healthy and have strong bone structure around the knee. Because bone cement can break away and cause an implant to loosen, cementless knee replacements are less likely to loosen over time.
For this reason, cemented knee replacements are considered better suited for older, less active patients.
Types of Knee Implants
There are multiple types of knee implants that doctors and patients can discuss before choosing the best option.
Regardless of type, all knee implants have certain things in common.
All consist of a component that attaches to the thigh bone and one that attaches to the tibia, one of the two lower leg bones. A knee replacement implant may or may not have a patellar component mimicking the kneecap.
Some components, particularly the bearings, may be made of ceramics or a mixture of ceramics and metal. The materials have to be “biocompatible,” meaning they cannot trigger the body’s rejection response. Knee implants are relatively lightweight — usually between 15 and 20 ounces.
Fixed Bearing
This is the implant most patients receive. Less mobile and not as strong as other implants, it is best suited for patients who are not overweight and who do not have an active lifestyle. It is usually recommended for elderly patients who will not put serious wear-and-tear on the implant.
Another component is attached to the femur, where it can roll on the polyethylene.
The drawback is that this contact causes wear on the polyethylene. Studies have shown that this stress is a leading cause of fixed bearing long-term implant failures. It wears away the polyethylene component, causing the implant to loosen. Loosening is not only painful, it is also a major cause of implant failure.
Studies have shown that 95% of fixed bearing implants continue to function properly 10 years after patients received them.
Mobile Bearing (rotating platform)
This design allows the plastic cushion of the tibial component to rotate, giving patients greater flexibility on the medial (inner) and lateral (outer) sides of the knee. Mobile bearing implants work well for young and active patients.
The polyethylene component in mobile bearing implants is designed to fit into the metal tibial tray component in a way that allows limited rotation. The design was introduced to limit the polyethylene wear seen in fixed-bearing designs. It produces less stress between components and in theory should reduce chances of — or at least delay — loosening.
Mobile bearing implants tend to have less stress between the femoral and tibial surfaces, granting the flexibility to benefit a patient’s gait and even deep knee bends. However, their long-term durability is about the same as for fixed bearing implants in older patients.
Like the fixed-bearing design, mobile bearing knee implants have a 95% survival rate 10 years after being implanted.
Medial Pivot (mobile bearing)
The medial pivot design incorporates a mobile bearing to more effectively replicate the natural function of the knee. It rotates, twists, bends and flexes like a natural knee joint. More complicated than fixed or standard mobile bearing designs, it can be more expensive.
Instead of a “hinge joint” approach used by more conventional knee replacements, the components of a medial pivot implant incorporate a “ball-and-socket” approach. It tends to be more stable than some other implant designs. Because it allows for a large contact area between components, it reduces wear-and-tear, extending the life-expectancy of the implant. But this design is more dependent on tissue and surrounding ligaments to prevent dislocation. This can result in tissue becoming caught in the implant, which can cause pain.
A 2017 study of 325 patients with a total of 347 medial pivot knee implants showed good long-term results for the design. Researchers conducted follow-ups with patients over an average of 15.2 years. They found that 98.8% of medial pivot implants survived to 17 years and 94% of patients were able to do age-appropriate activities, with an average knee bend of 120 degrees, in their final follow-up sessions.
Posterior Cruciate Ligament (PCL) Retaining (nonconstrained)
The posterior cruciate ligament (PCL) runs along the back of the knee, connecting the femur to the tibia. This design keeps the PCL intact, but it depends on several patient factors: good bone quality, few defects in the bones, intact soft tissue around the knee and a functional PCL.
There are two types of PCL implants: retaining and substituting. The difference between the two comes in part from how the PCL is affected by the implant surgery. A surgeon may remove the ligament to implant a PCL substituting implant. But if the ligament is in good condition, the surgeon may want to preserve it. In that case, he or she will use a PCL retaining implant.
Preserving the ligament may not necessarily result in better postoperative knee function. A simple polyethylene bearing attaches to a metal component implanted in the tibia, and a metal implant in the femur hinges on the polyethylene. It is a minimal design dependent on the PCL to stabilize the implant, but a tight PCL may lead to excessive wear on the bearing.
Less bone is removed with a PCL retaining implant. A PCL retaining implant is less likely than a PCL substituting version to result in a condition called “patella clunk” syndrome. This syndrome results from scar tissue forming near the implant and becoming caught in part of the device as the knee is fully extended.
A 2015 study reviewed 15 years of follow-ups of patients who had received PCL retaining implants. It found 98.7% of the implants survived 10 years and 83.6% survived 17 years.
Posterior Cruciate Ligament (PCL) Substituting (constrained)
This design replaces ligament with plastic components. It is recommended primarily for patients with severely damaged knees or weak ligaments. Also used in revision surgery.
It is indicated for patients with severe knee deformities or who have had previous knee replacement surgery or have had a knee cap removed.
The PCL substituting design has a tall post attached to the tibia that fits into a deep box attached to the femur. The two are not connected with any kind of hinge joint. A polyethylene bearing attaches to the tibial component.
A 2016 study of the PCL substituting design found that 88.5% of PCL substituting implants used in initial knee replacement surgery survived 10 years. For revision surgery, the 10-year survival rate was 75.8% if the revision surgery was due to some cause other than infection, and 54.6% if revision was due to infection.
Gender Specific
Women undergo more knee replacements than men – accounting for roughly two-thirds of all knee replacement surgeries in the U.S. Surgeons performing knee replacements have long reported anatomical differences between men and women, which make a “one-size-fits-all” approach ineffective in knee replacement surgery.
“Female anatomy is a little different,” Dr. Anthony Unger, a surgeon who has performed hundreds of knee replacements, told National Public Radio in 2007. “The end of the bone called the femur (thigh) is a little different contour.”
Some women may be shorter or have smaller body frames than the overall population. Gender-specific implants, engineered to the various different dimensions of male and female body frames, are designed to perform better for specific patients.
Differences Between Total and Partial Knee Replacement
Knee replacement surgery is recommended when conservative treatments such as physical therapy, braces, steroid injections and anti-inflammatory medication fail to alleviate pain.
If a patient requires surgery on both knees, it’s called a bilateral knee replacement. The two procedures can be done simultaneously or doctors may choose to use a staged bilateral approach that schedules the second surgery several days, weeks or months later.
The decision to have a total versus a partial knee replacement is based on a doctor’s recommendation after a full patient evaluation is performed.
Total Knee Replacement

A total knee replacement is actually the resurfacing of the bones in all three compartments of the knee joint: The medial compartment, the lateral compartment and the patellofemoral (front) compartment.
The procedure resurfaces the end of the femur, the top of the tibia, and the patella. The ligaments that support the knee can be left in place or removed, depending on their condition and the type of implant chosen. Any existing cartilage between the femur and tibia is replaced with a plastic cushion.
Partial Knee Replacement

A partial knee replacement is a procedure that resurfaces one (unicompartmental) or two (bicompartmental) sides of the knee. Partial implant components are named for the area of the knee they resurface: Medial unicondylar component, lateral unicondylar component and patellofemoral component.
A patellofemoral surgery replaces the end of the thigh bone with a metal piece and resurfaces the back of the patella. A partial knee replacement can also include a knee osteotomy, in which a surgeon removes or adds a wedge of bone to the tibia or femur to take some of the weight off of the damaged part of the knee.
Common and Serious Complications of Knee Replacement
While knee implants give many recipients a second chance at walking and living a more normal life, complications do occur.
Most problematic is a loosening of the implant, which can be caused by a defective implant or poor positioning at the time of surgery. Implant loosening is a primary cause for revision surgery.
Although rare, metallosis is possible after knee replacement surgery. Metallosis, also known as metal poisoning, can occur when metal implant pieces rub against each other and release tiny metal particles into the knee joint and bloodstream.
- Blood clots
- Nerve and tissue damage
- Pain and soreness
- Swelling and stiffness
This can happen when the plastic cushion separating the femoral and tibial components wears down from high usage. This usually takes a few years to occur, and revision surgery is required.
Joint infection is also rare — occurring in less than 2% of patients — but is considered one of the most serious complications following knee replacement surgery. Infections are usually related to sterility issues and the hospital where the surgery takes place.
Many of these common complications go away or significantly improve within a couple of weeks, and rehabilitation after surgery typically lasts several months. But some complications can require revision surgery to correct. Patients may need surgery to remove the infection or to replace defective implants. Thousands of people have filed knee replacement lawsuits over these serious complications.
Expected Lifespan and Need for Revision Surgery
Knee replacements generally last at least 15 years and can last far beyond 20 years, but not all patients experience the same results.
For patients whose artificial joint wears out earlier than expected — or who received a defective implant — revision surgery is required. Any serious complication can also lead to revision surgery. In addition, younger recipients require revision surgery when the first implant wears out.
- Bleeding
- Blood clots
- Bone fracture during surgery
- Infection in the wound or the new prosthesis
- Heart attack, stroke or lung complications (rare)
- Poor wound healing
Revision surgery rates for knee replacements are quickly rising. In 2010, more than 55,000 revision surgeries were performed in the U.S., with 48% of the revisions in patients under 65. Total costs for each surgery averaged to be more than $49,000.
By 2030, estimates predict there will be nearly 275,000 procedures performed each year — a 500% increase from 2010, when there were approximately 55,000 knee replacement revisions.
Implants used in revision surgeries typically have thicker, longer stems for added stability and to replace bone loss. In addition, surgeons typically implant a constrained (hinged) knee during revision surgery because it provides strength for severely damaged knees and weak ligaments. The vast majority of these procedures result in favorable long-term outcomes. However, as with any surgery, there is a risk of complications.
Knee Implant Manufacturers and Models
There are well over a dozen knee replacement manufacturers in the U.S., but most of the market is dominated by four companies, each making several models of implants.
Zimmer-Biomet
Zimmer and Biomet merged in 2015 and together dominate the global hip and knee replacement market with about a 35% share. The company produces roughly 25% of all knee implants worldwide. It makes implants for total knee replacement, partial replacement, revision surgery components and other products to preserve or repair damaged knees.
- Zimmer Persona
- Total knee replacement. The latest generation of Zimmer-Biomet knee replacement implants, the Personal was built on past Zimmer technology with the goal of better mimicking natural knee motion.
- Zimmer NexGen
- Total knee replacement and revision systems.
- Gender Solutions
- Total, partial, and revision knee replacement systems. Different designs take into account men’s and women’s physiology to fit better with patient anatomy.
- Vanguard Individualized Design
- Total, partial, and revision knee replacement systems. This line is manufactured in many different sizes to allow more individualized fit for patients.
- Oxford
- Partial knee system. Manufactured for more than 35 years, Zimmer-Biomet claims that the Oxford system is the most widely used partial knee implant in the world.
DePuy Synthes
This Johnson & Johnson subsidiary is the second-largest hip and knee implant manufacturer in the world. It had an estimated $1.5 billion in sales of knee replacements for 2016.
- Attune
- Total and revision knee replacement systems. DePuy’s latest generation knee replacement.
- Sigma
- Total and partial knee replacement systems. Manufactured in both mobile and fixed bearing versions.
- S-ROM Noiles
- Total and revision knee replacement. This rotating, hinge knee system is designed for patients with severe bone deficiency or soft tissue instability.
- LCS Complete
- Total knee replacement and revision replacement systems. Evolving from DePuy’s original design from the 1970s, this device is manufactured in both mobile and fixed bearing designs.
Stryker Corporation
Stryker Corporation reported nearly $1.5 billion in sales of its knee implants for 2016. That was 34% of all implant sales for the company and the most for any joint replacement the company manufactured. Stryker received U.S. Food and Drug Administration approval for its Mako robotic arm, assisted-knee implant technology in 2015 and has reported strong sales of the devices, which help surgeons plan and carry out knee implant surgery.
- Triathlon
- Total, partial and revision knee replacement systems. Features 150-degree range of movement.
- Triathlon Tritanium
- Total knee system. A cementless implant that incorporates porous design features to allow bone to integrate with bone.
- Scorpio
- Total and revision knee replacement systems. Stryker claims more than a half-million Scorpio systems have been implanted worldwide.
- Duracon TS
- Revision knee replacement system.
- Avon Patello-Femoral
- Partial knee replacement. Designed for patients with specific arthritic condition affecting the area of the kneecap and femur.
Smith & Nephew
UK-based Smith & Nephew reported $932 million in revenue from its knee implants in 2016. The company also introduced its first robotic knee implant procedures using its newly acquired NAVIO system that same year. Some Smith & Nephew knee replacements use a proprietary oxidized zirconium bearing the company claims has less wear than plastic ones.
- Journey I BCS
- Total and partial knee replacement systems. This line was marketed to younger, more active patients. The product was phased out in 2013 and 2014, and recalled in 2018.
- Journey II
- Total and partial knee replacement systems. This line is marketed particularly toward younger, “active” knee replacement candidates.
- Genesis II
- Total knee replacement system. Smith & Nephew has manufactured different versions in this line since the 1990s currently in PCL substituting or retaining versions. It is part of the company’s Legion series.
- Legion
- Total knee replacement and revision systems. Implants are made in PCL substituting and retaining versions and a hinged knee to provide greater stability if ligaments are unable to support the implant.
Arthrex Inc.
Florida-based medical device manufacturer Arthrex Inc. manufactures several products to treat various knee problems, including torn ligaments and cartilage damage. The iBalance line is its flagship line for total and partial knee replacements. The company made $2 billion in annual revenue in 2017, according to Forbes.
- Arthrex iBalance Total Knee Arthroplasty
- The total knee replacement system comes with a variety of sizes and accommodates male and female anatomy with easy-to-use, customizable instruments for surgeons.
- Arthrex iBalance Unicondylar Knee Arthroplasty
- The partial knee replacement system repairs one compartment of the knee joint and spares as much normal tissue as possible. Surgeons have the option to use a proprietary graft system to preserve ligaments and stimulate bone marrow growth.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

