Depakote
Depakote (divalproex sodium) is an anticonvulsant medication. Doctors prescribe it to treat seizure disorders, prevent migraine headaches and manage bipolar disorder. Depakote side effects can be serious and sometimes fatal. These include birth defects in children whose mothers take it while pregnant.
- Medically reviewed by Jessica D. Hess, Ph.D.
- Last update: March 10, 2025
What Is Depakote?
Depakote (divalproex sodium) is an anticonvulsant. Doctors prescribe it to treat conditions that affect the brain. It contains the active ingredient divalproex sodium, which is a combination of sodium valproate and valproic acid.
The medication comes in a white powder form. Drugmaker AbbVie Inc. makes it into a tablet. Patients take Depakote by mouth. The drug’s maker tells patients to swallow Depakote whole, not to crush or chew it.
Valproate in Depakote is effective in managing and stabilizing moods, but the chemical substance can cause serious side effects. Depakote lawsuits blame the drug for causing birth defects in children whose mothers took Depakote during pregnancy.
Depakote Uses
The U.S. Food and Drug Administration approved Depakote in 1983 to treat epilepsy. Doctors may sometimes prescribe divalproex sodium with other medications to treat types of seizures.
The FDA expanded Depakote uses to include the treatment of manic episodes associated with bipolar disorder. Divalproex sodium also helps prevent migraines headaches.
What Depakote Does for the Brain
Divalproex sodium works by increasing the amount of gamma-aminobutyric acid (GABA) in the brain. The body produces GABA naturally. It is a chemical neurotransmitter — or brain messenger.
Faster than normal electrical impulses in the brain can cause erratic impulses. These impulses overstimulate the nerves. GABA helps to calm and relax nerves. Relaxing nerves can stabilize moods. Increasing GABA can also prevent abnormal brain signals that lead to seizures.
One 2022 clinical research trial reported on the effects of Depakote on posttraumatic irritability after traumatic brain injury. Results showed a significant and sustained reduction of posttraumatic irritability. However, the study authors noted that treatment efficacy was not related to measures of anxiety, posttraumatic stress disorder, sedation, or veteran versus nonveteran status. Alcohol use did not change as a result of treatment.
Types of Depakote
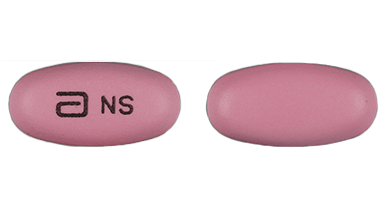
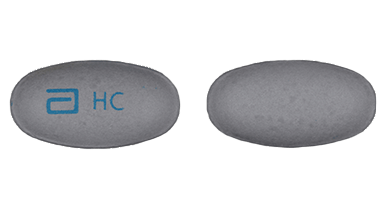
Divalproex sodium comes in Depakote tablets and Depakote ER (extended-release) tablets. It’s also available in Depakote Sprinkle Capsules (delayed-release capsules). Depakote ER and the delayed-release formulation of Depakote are not interchangeable.
Depakote tablets are delayed release. They have a coating to keep the medication from dissolving too soon after it’s swallowed. These tablets come in three sizes: 125 mg, 250 mg and 500 mg. They are prescribed to be taken twice a day.

Depakote ER tablets are made to slowly deliver the medication over 24 hours. They are taken just once a day. They come in 250 mg and 500 mg. Depakote ER has a coating designed to slowly deliver the medication over 24 hours.

Depakote Sprinkle Capsules are approved only for the treatment of epilepsy. They are available in 125 mg. They work similar to Depakote delayed release, except that they are in capsules rather than tablets. Patients who have trouble swallowing may open the capsules and sprinkle the medication on soft food.
A closely related medication, Depakene (valproic acid), comes in capsule and liquid form. Another variety of valproic acid, Stavzor, is no longer manufactured. In 2008, the FDA approved the first generic version of Depakote. Collectively, these medications are known as valproate products.
Depakote Dosages
Depakote dosage can vary. It depends on the patient and the condition for which a doctor prescribes it. For example, when taken to control mania, the recommended initial dose is 750 mg a day taken in divided doses for Depakote. For Depakote ER, the recommended initial dose is 25 mg/kg once a day, up to a maximum of 60 mg/kg a day.
The initial Depakote therapy is 10 mg/kg to 15 mg/kg for treating epilepsy in patients aged 10 and older. Doctors can then increase the dosage by 5 mg/kg to 10 mg/kg each week. This continues until the doctor determines that the medication is doing what it’s supposed to. With Depakote ER, patients ages 10 and older should start the same with a maximum dose of 60 mg/kg a day.
If a patient forgets to take Depakote at the usual time, he or she can take it upon remembering. But if it’s close to the next dose, patients can skip the forgotten dose and resume the normal schedule. Do not double up.
Depakote Interactions
Valproic acid in Depakote may interact with a number of different medications. Depakote interactions may increase or decrease the effects of the medications. Some can be fatal.
Valproic acid can increase the serum concentrations of diazepam in patients taking that medication. Antacids containing magnesium and aluminum hydroxide may increase valproic acid by an average of 12%.
Patients with urea cycle disorders who are being treated with sodium phenylbutyrate should not receive valproic acid. This interaction can be fatal. Supplements and food can also interact with Depakote. For example, high doses of folate can decrease the effectiveness of Depakote. High doses of the herb Ginkgo biloba also could decrease the effectiveness of Depakote.
- Aspirin
- Amitriptyline
- Alprazolam
- Bupropion
- Butabarbital
- Carbamazepine
- Cannabidiol
- Cholestyramine
- Clonazepam
- Diazepam
- Doripenem
- Ertapenem
- Estrogen-containing birth control
- Ethosuximide
- Felbamate
- Haloperidol
- Lamotrigine
- Loxapine
- Meropenem
- Methotrexate
- Nortriptyline
- Pemoline
- Phenobarbital
- Phenytoin
- Propofol
- Rifampin
- Ritonavir
- Rufinamide
- Sodium Phenylbutyrate
- Thiothixene
- Tolbutamide
- Topiramate
- Vorinostat
- Warfarin
- Zidovudine
Common Side Effects of Depakote
A common side effect of Depakote and Depakene is nausea, especially during the first month of treatment. This can be overcome by starting on a low dosage and slowly increasing the amount. Taking the medication on a full stomach can also help.
- Abdominal pain
- Diarrhea
- Drowsiness
- Hair loss
- Nausea
- Low platelet count
- Tremors
- Vomiting
These side effects may be mild or moderate. You should talk to your doctor about any side effects because they could be signs of something serious.
Depakote Serious Side Effects
Taking Depakote has been linked to some serious and even deadly side effects. Liver damage is one of the side effects that may be fatal. This is especially true in children under 2. This risk is highest in the first months of taking the medication. The risk may still be present even after the Depakote medication is stopped.
Another potentially fatal side effect is inflammation of the pancreas, or pancreatitis. This is when digestive enzymes start digesting the pancreas itself.
When pregnant women take Depakote, their unborn babies are at risk of developing birth defects. These defects can affect the brain, spinal cord, heart, arms, legs and penis. These babies also risk developing lower intelligence. Women who are or may become pregnant should not take Depakote.

Depakote Black Box Warnings
The FDA required that Depakote’s label have black box warnings, now called boxed warnings. A boxed warning is the agency’s most serious type of warning. It calls attention to serious or life-threatening risks.
Depakote’s boxed warnings are for hepatotoxicity, fetal risk and pancreatitis.
Depakote Precautions
Depakote manufacturer AbbVie warns that certain people should not take Depakote or Depakene. This includes people with liver problems, and women who are or may become pregnant.
Talk to your doctor before taking Depakote or Depakene if you:
- Have liver problems
- Have or think you have a genetic liver problem caused by a mitochondrial disorder (e.g. Alpers-Huttenlocher syndrome)
- Are allergic to divalproex sodium, valproic acid, sodium valproate, or any of the ingredients in Depakote or Depakene
- Have a genetic problem called urea cycle disorder
- Are or may become pregnant
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


