Fosamax Safety, Side Effects and FDA Warnings
Fosamax (alendronate sodium) treats osteoporosis and Paget's disease, and it has been associated with serious side effects such as osteonecrosis of the jaw (ONJ) and femur fractures. This led to FDA warnings and injury lawsuits.
- Last update: June 24, 2025
What Is Fosamax and How Does It Work?
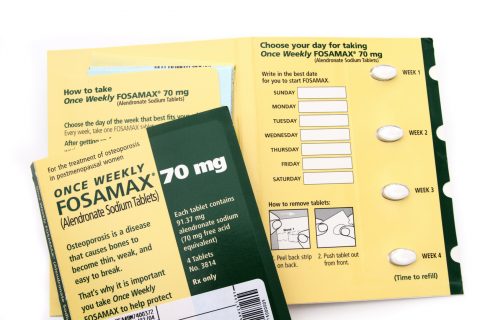
Fosamax is the brand name for alendronate sodium, a prescription medication primarily used to prevent and treat osteoporosis — a condition that causes bones to become weak and brittle — in men and postmenopausal women. It’s also used to treat Paget’s disease of bone, a disorder that results in weak, soft bones.
The drug was first approved in 1995, and it belongs to a drug class called bisphosphonates. Fosamax works by altering the process of bone breakdown to help slow bone loss, increase bone density and prevent bone fractures.
Organon is the drug’s current manufacturer, and before that, Merck manufactured it.
Common and Serious Side Effects of Fosamax
Common, less serious side effects of Fosamax include abdominal pain and joint pain, while serious side effects include bone problems and esophagus problems.
In clinical trials, the most common side effects occurred in three percent or more of trial participants.
- Constipation
- Diarrhea
- Heartburn
- Nausea
- Pain in your bones, joints or muscles
- Stomach area (abdominal) pain
- Upset stomach
Common side effects may last anywhere from a few days to a few weeks. Make sure to let your medical provider know if you experience any side effects.
Serious Fosamax Side Effects: Jawbone, Thigh Bone and Esophagus Problems
Three of the most serious Fosamax side effects include problems with the jawbone, thigh bones – also called femurs – and the esophagus.
Osteonecrosis of the jaw, or ONJ, is a serious condition where the gums don’t cover the jawbone, and the bone weakens and dies. While the risk of ONJ is generally low, it is higher in people who take Fosamax. The risk is even higher if a person has invasive dental work, such as a dental implant or extraction, while taking Fosamax.
Fosamax is also associated with increased reports of thigh bone fractures that may occur with long-term use of the drug. These fractures occur just below the hip joint in the upper part of the thigh bone.
Patients have reported problems with esophageal irritation, such as ulcers or bleeding. In some cases, patients had to go to the hospital.
People who suffered from ONJ and thigh bone fractures filed Fosamax lawsuits alleging that the manufacturers didn’t properly warn about the risks. While the ONJ cases were settled in 2013 for $27.7 million, 950 femur fracture cases remain pending in New Jersey multidistrict litigation under MDL 2243 as of May 2025.
Bones naturally go through a cycle of breaking down and rebuilding to stay strong. Fosamax slows bone breakdown, which over time may disrupt the cycle and indirectly reduce new bone growth. This could explain why long-term use has been linked to fractures in some people.
One Woman’s Experience with Fosamax
One patient, identified by her initials C.H. to protect her privacy, told Drugwatch that she suffered ONJ and a thigh bone fracture after taking Fosamax. She has had multiple surgeries and filed a Fosamax lawsuit.
“I didn’t understand until I looked into it more and had a professional explain it to me … Fosamax was supposed to make my bones stronger. In fact, what it does is make them brittle,” she said.
FDA Warnings and Label Changes
The FDA required Fosamax label changes to warn of ONJ and femur fractures.
Merck first added a warning about ONJ to Fosamax’s label in 2005. The company did so after the FDA cited increasing reports of ONJ in 2004 and urged the drugmaker to make label changes. In 2010, the FDA required Merck to add warnings about thigh fractures (atypical femur fractures) to the Warnings and Precautions section of Fosamax’s drug label.
Fosamax has been on the market since 1995. Because the ONJ and thigh fracture warnings were not added until 2005 and 2010, respectively, patients and doctors were unaware of these risks for many years.
Fosamax doesn’t have any black box warning for serious side effects that may cause serious harm or death.
Is Fosamax Still Considered Safe?
In general, Fosamax is still considered safe with a small risk of ONJ and femur fractures. Fosamax is still available in the U.S. in its brand name and generic forms.
The FDA hasn’t released any information on the ideal duration of Fosamax treatment. At the time of the agency’s 2010 safety communication, evidence showed bisphosphonates were effective at reducing fractures for at least three years, and in some cases, for five years.
A study in JAMA found that the benefits of women taking bisphosphonates tapered off by year seven. Study authors said scientists need to do more research on discontinuation times. This could mean that patients may avoid the potential risk of femur fracture or ONJ by stopping the drug after the benefits taper off.
Another review from Stat Pearls suggested giving patients a break from Fosamax treatment. Patients with a low fracture risk could take this break, known as a “drug holiday,” for three to five years. Though for some, the benefits of continued therapy outweigh the risk of side effects. The review authors suggest patients should have follow-up assessments to measure their bone density and calcium levels at six to 12 months after starting treatment.
Make sure you discuss monitoring your condition with your medical provider.
Has Fosamax Been Recalled?
Fosamax has not been recalled in the U.S. The FDA said it would monitor any data regarding femur fracture risk in 2010, but there haven’t been any follow-up reports.
What Should You Do If You're Experiencing Side Effects?
If you are experiencing side effects, make sure you talk to your medical provider. If you have new thigh or groin pain, it could be a sign of a femur fracture, and you should tell your medical provider right away. Your medical provider may recommend tests, such as X-rays, to rule out a femur fracture.
ONJ symptoms can last for 8 weeks or longer and include pain and swelling in the mouth, as well as part of the jawbone showing through the gums. Your dentist should monitor these symptoms.
You and your doctor can report any side effects to the FDA through its MedWatch Program.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.