Pradaxa
Pradaxa (dabigatran) is a prescription anticoagulant, or blood thinner, designed to reduce the risk of stroke and blood clots. It's widely used as an alternative to warfarin for patients with heart and clotting disorders such as non-valvular atrial fibrillation, deep vein thrombosis (DVT) or pulmonary embolism (PE). Complications such as uncontrolled bleeding, gastrointestinal hemorrhages and brain bleeding have prompted FDA warnings and label updates.
Our content is developed and backed by respected legal, medical and scientific experts. More than 30 contributors, including product liability attorneys and board-certified physicians, have reviewed our website to ensure it’s medically sound and legally accurate.
legal help when you need it most.
Drugwatch has provided people injured by harmful drugs and devices with reliable answers and experienced legal help since 2009. Brought to you by The Wilson Firm LLP, we've pursued justice for more than 20,000 families and secured $324 million in settlements and verdicts against negligent manufacturers.
More than 30 contributors, including mass tort attorneys and board-certified doctors, have reviewed our website and added their unique perspectives to ensure you get the most updated and highest quality information.
Drugwatch.com is AACI-certified as a trusted medical content website and is produced by lawyers, a patient advocate and award-winning journalists whose affiliations include the American Bar Association and the American Medical Writers Association.
About Drugwatch.com
- 15+ Years of Advocacy
- $324 Million Recovered for Clients
- 20,000 Families Helped
- A+ BBB Rating
- 4.9 Stars from Google Reviews
Testimonials
I found Drugwatch to be very helpful with finding the right lawyers. We had the opportunity to share our story as well, so that more people can be aware of NEC. We are forever grateful for them.
- Medically reviewed by Kenneth S. Fill, Pharm.D., MBA
- Last update: November 10, 2025
- Est. Read Time: 7 min read
What Is Pradaxa and Who Takes It?
Pradaxa is a direct thrombin inhibitor that helps reduce the formation of blood clots, especially in people with an irregular pulse (atrial fibrillation) that is not caused by a heart valve problem. The medication works by blocking thrombin, a key enzyme involved in the blood clotting process.
Pradaxa received FDA approval in October 2010 for stroke prevention in atrial fibrillation (AF) patients, and in 2015, the medication was also approved for treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE). Doctors have written more than 17 million Pradaxa prescriptions in the United States.
Initially, Pradaxa was widely embraced by medical professionals and patients as a convenient alternative to warfarin, which had been the only oral anticoagulant available in the United States for stroke reduction. Unlike with warfarin, patients taking Pradaxa are not required to undergo regular blood tests or maintain a strict diet.
Pradaxa Side Effects: Common and Severe Risks
Bleeding, sometimes serious, is the most common side effect of Pradaxa. A fair number of patients taking Pradaxa experience adverse gastrointestinal effects. These include abdominal pain, gastritis, gastroesophageal reflux disease (GERD) and gastric bleeding.
- Abdominal pain
- Bleeding
- Nausea
- Stomach inflammation
- Tiredness
- Upset stomach
- Vomiting
As of Oct. 28, 2025, bleeding and stroke were the most common Pradaxa side effects reported to the FDA. Gastrointestinal bleeding was the most commonly reported type of bleeding. Falls, anemia, and rectal bleeding were other reported adverse reactions.
Most adverse events reported to the FDA were serious. The number of reported problems peaked in 2011 and remained high through 2014. This coincides with the release of FDA safety warnings for many of the side effects.
| FDA Adverse Events Reporting System (FAERS) Data for Pradaxa Side Effects, 2025 | |
|---|---|
| Total cases reported | 63,604 |
| Serious cases (including deaths) | 48,438 |
| Deaths | 9,805 |
In clinical trials, gastrointestinal bleeding was more common among patients taking Pradaxa compared to those on warfarin.
“To minimize the gastrointestinal issues, Pradaxa can be taken with meals,” clinical pharmacist Kenneth S. Fill told Drugwatch. “Be extra cautious during physical activities to reduce the chance of minor or major bruising.”
Serious Side Effects
Bleeding risks, such as hemorrhaging, gastrointestinal bleeding and stroke, are serious potential Pradaxa side effects. Gastrointestinal and internal eye bleeding were the most common types of bleeding reported in clinical trials.
There is also a risk of hematomas (pooled blood). In rare cases, patients reported severe allergic reactions, including anaphylaxis, when taking Pradaxa.
“Signs and symptoms to look out for include unusual or prolonged bleeding, excessive bruising, and blood in the urine or stool,” Fill said.
Notify your doctor immediately if you notice any symptoms of bleeding disorders, such as bleeding from your gums, frequent nosebleeds or heavy periods. However, you generally shouldn’t stop taking Pradaxa without speaking to your doctor.
“Stopping Pradaxa abruptly can lead to a rebound effect where the risk of blood clots increases,” Fill said. “This is particularly dangerous for those that are prone to or at a high risk of stroke or thromboembolism.”
- Blood Clots
- Patients have an increased risk of developing blood clots when they stop taking Pradaxa. This can cause severe complications, including stroke and death. The most recent FDA review indicates this risk is lower than early studies suggested, but it is still a concern.
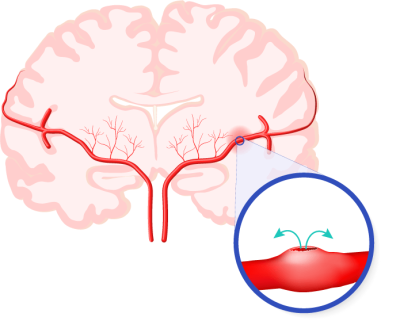
- Brain Bleeds
- Rarely, Pradaxa increases the risk of brain bleeds, which can cause life-threatening and/or permanent brain damage.
- Gastrointestinal Hemorrhaging
- Researchers found that higher doses of Pradaxa (and other dabigatran drugs) could create an increased risk of GI bleeding compared with warfarin.
- Spinal or Epidural Hematomas
- Epidural or spinal hematomas can occur in patients treated with Pradaxa who receive epidural or spinal punctures. These punctures may be performed for medical reasons, such as administering an anesthetic. A hematoma is a collection of blood that pools in your tissue, forming a solid swelling or mass. A hematoma near the spine, especially in the epidural space, can lead to paralysis if left untreated.
- Uncontrolled Bleeding
- The FDA indicates that Pradaxa can cause significant and sometimes fatal bleeding. In general, major bleeds were found to be more common among those taking Pradaxa. In a study of 9,404 participants from the Journal of JAMA Internal Medicine, 9% of Pradaxa users experienced a major bleed, compared with 6% of warfarin users.
Before the development of Pradaxa reversal agents — substances that can counter the effects of another drug — there was no means to truly combat the effects of Pradaxa. Warfarin, on the other hand, already had a reversal agent. Many people died as a result of uncontrolled bleeding when medical care providers were unable to do anything to stop it.
Case Study: John Wilchinski's Cerebral Hemorrhage After Pradaxa Use
John Thomas Wilchinski, a resident of Greenville County, Tennessee, was prescribed Pradaxa in February 2011. After just two months of use, he suffered a severe cerebral hemorrhage (a life-threatening type of bleeding in the brain), according to court documents. This serious side effect has had lasting impacts on his health and well-being.
Permanent Injuries
As a result of the cerebral hemorrhage caused by Pradaxa, Wilchinski faced permanent injuries. These include ongoing physical pain, mental anguish and diminished enjoyment of life. His condition requires lifelong medical treatment and continuous monitoring.
Ongoing Health Concerns
The side effects of Pradaxa left Wilchinski with a fear of future health complications. His experience highlights the significant risks associated with Pradaxa. The risk was compounded by the lack of a reversal agent at the time of his cerebral hemorrhage, making managing his bleeding events extremely difficult. While Pradaxa now has an antidote called idarucizumab, the FDA didn’t approve its use until 2015. Wilchinski’s incident occurred in 2012.
FDA Black Box Warning and Label Revisions
The boxed warning for Pradaxa’s prescribing information covers two conditions: thrombotic events and epidural or spinal hematomas. Boxed warnings are the most serious drug label warning the FDA issues.
Because there is an increased risk of blood clots among patients who discontinue treatment with Pradaxa, the boxed warning cautions against stopping an anticoagulant without replacing it with another medication.
Additionally, in patients taking Pradaxa, blood may pool against the spine during spinal punctures and certain types of spinal anesthesia. This condition, called a spinal hematoma, can lead to permanent paralysis.
- Thrombotic events (blood clots that block a blood vessel), if they stop taking the drug prematurely.
- Spinal/epidural hematomas (a collection of blood in the area between the spine's protective covering and the vertebrae), which could occur in patients receiving neuraxial anesthesia or undergoing spinal puncture. Permanent paralysis could result.
The FDA issued a Drug Safety Communication on December 7, 2011, alerting consumers to reports about significant bleeding in Pradaxa users. There have been numerous additional FDA communications since then, including but not limited to the following:
-
2012
The FDA warned that Pradaxa shouldn't be used to prevent stroke or blood clots in patients with mechanical heart valves.
-
2013
The FDA added a black box warning about an increased risk of thrombotic events (clotting) if a patient abruptly discontinues the medication.
-
2014
The FDA added a black box warning about the risk of spinal or epidural hematomas for patients on Pradaxa who receive a spinal puncture.
-
2014
The FDA found that the risk of stroke was lower with Pradaxa than with warfarin, but the risk of major gastrointestinal bleeding was higher.
There is mixed evidence on how Pradaxa compares to other blood thinners. A 2019 study in The American Journal of Medicine examined the safety profiles of several blood thinners in Medicare patients. The results showed a slightly decreased risk of internal bleeding in the brain or skull when taking Pradaxa compared to similar medications.
However, a 2021 meta-analysis published in Frontiers in Pharmacology found that Pradaxa has an increased rate of gastrointestinal bleeding. Before that, a 2014 article from the Journal of the American Heart Association found that patients on dabigatran, the active ingredient in Pradaxa, have a 33% increased risk of heart attack compared to warfarin users.
Careful monitoring can reduce the dangers of major bleeding and related complications.
Reversal Agents for Pradaxa Bleeding
When Pradaxa came onto the market, there were no reversal agents. This means there was no effective way to stop uncontrolled bleeding caused by Pradaxa.
In 2015, the FDA granted accelerated approval for a drug called Praxbind (idarucizumab), which was the first reversal agent for Pradaxa-related bleeding. When preliminary evidence suggests a drug can address a medical need that other approved medications can’t, it may be granted accelerated approval to meet that demand. Although accelerated approval requires less evidence than the typical approval process, Praxbind did get full approval in 2018.
Praxbind works by binding to dabigatran and neutralizing its anticoagulant effects within minutes. This medication can be used when a patient taking Pradaxa requires emergency surgery or develops uncontrolled bleeding.
Despite Praxbind’s use as an emergency option, it did not eliminate legal concerns nor help the patients and families who had been affected by Pradaxa-related complications before the release of Praxbind.
Pradaxa Recalls and Safety Alerts
Despite the risks associated with Pradaxa, the medication was never recalled because of them.
While a 2012 FDA recall did occur, it was prompted by a packaging defect that could have compromised the integrity of the drug by allowing moisture to get into the packaging. This recall only affected one lot of the medication.
In 2023, Ascend Laboratories LLC. also recalled Dabigatran Etexilate Capsules due to elevated levels of N-Nitroso-dabigatran. Although this chemical is common and even found in places like drinking water and vegetables, high doses can potentially cause cancer. The recalled capsules included a generic version of Pradaxa.
Lawsuits Over Pradaxa’s Risks
Pradaxa’s manufacturer, Boehringer Ingelheim Pharmaceuticals, was sued by thousands of patients for allegedly failing to disclose the risk of severe complications. In their Pradaxa lawsuits, plaintiffs claimed that the company:
- Engaged in deceptive marketing and misled patients and doctors about the dangers of Pradaxa.
- Failed to provide adequate warning of the bleeding risks.
- Developed an antidote but did not seek approval for the reversal agent until 2015.
Boehringer Ingelheim Pharmaceuticals settled the majority of claims in 2014 and the remainder of the claims in 2020. The company paid out $650 million in settlements, with an average compensation of around $160,000 per person.
What Patients Should Know and Do Next
Patients who use Pradaxa should consult their doctors if they experience any unusual symptoms, including unexplained bruising, bloody urine or fatigue. These symptoms could be a sign of internal bleeding or other complications. Patients are also advised to monitor both kidney function and clotting parameters, especially if they are long-term Pradaxa users.
If patients experience complications, they should report them to the FDA’s MedWatch program. Speaking with an experienced attorney can help you understand your legal options if you suffered harm from Pradaxa.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.




