Xeljanz
Pfizer’s Xeljanz (tofacitinib) is used to treat rheumatoid arthritis and psoriatic arthritis. Xeljanz can also be used to treat symptoms of ulcerative colitis by lowering inflammation. The FDA has warned that taking high doses of Xeljanz can increase the risk of blood clots in the lungs and death.
- Medically reviewed by Amanda Gerberich, Pharm.D. BCPS
- Last update: March 13, 2025
What Is Xeljanz?
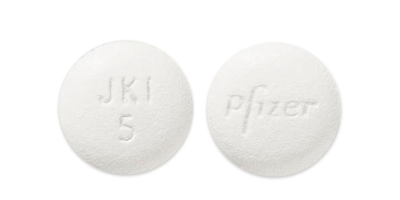
Xeljanz is an oral prescription medication approved to treat moderately to severely active rheumatoid arthritis, psoriatic arthritis and ulcerative colitis. It also comes in an extended-release formulation, Xeljanz XR.
Both formulations contain the active ingredient tofacitinib. The medication belongs to a class of drugs known as Janus kinase inhibitors, or JAK inhibitors.
Pfizer first gained U.S. Food and Drug Administration approval to sell Xeljanz in the United States in 2012. Since its release, the drug has become a blockbuster for Pfizer. In 2018, it brought in about $1.8 billion worldwide.
As of 2022, more than 80 countries have approved the medication for the treatment of rheumatoid arthritis. In addition, more than 40 countries approved it for the treatment of active psoriatic arthritis and 70 countries approved it for the treatment of ulcerative colitis.
From January 2013 to October 2018, doctors prescribed the drug to more than 140,000 people to treat their rheumatoid arthritis, according to the Xeljanz website.
| TREATMENT | XELJANZ | XELJANZ XR |
|---|---|---|
| HOW IT'S TAKEN |  |  |
| DOSAGE | 5 mg or 10 mg tablet | 11 mg extended-release tablets |
| HOW IT'S DELIVERED | Immediate-release tablet that releases medication into the body over the course of several hours | Extended-release tablet that releases medication into the body over the course of a day |
| CAN BE TAKEN WITHOUT METHOTREXATE | Yes | Yes |
Xeljanz Side Effects and Black Box Warning
Despite its popularity, the drug may cause a number of side effects. The Xeljanz side effects reported most often during the first three months of rheumatoid arthritis clinical trials were upper respiratory tract infection, cold-like symptoms, diarrhea, headache and high blood pressure. People who participated in ulcerative colitis clinical trials also reported rashes, Herpes zoster (shingles) and elevated cholesterol levels.
In September 2021 the FDA concluded: “There is an increased risk of serious heart-related events such as heart attack or stroke, cancer, blood clots and death with the arthritis and ulcerative colitis medicines Xeljanz and Xeljanz XR (active ingredient tofacitinib).” Based on these findings from clinical trials that compared Xeljanz to TNF blockers for rheumatoid arthritis, the FDA required a new, stronger boxed warning for Xeljanz.
The FDA notified the public in December 2021 that Xeljanz now carries a black box warning for serious infections, a higher rate of lymphoma and lung cancers, a higher rate of death, a higher rate of cardiovascular events (stroke, cardiovascular death and heart attack) and blood clots. The agency also limited the drug’s use to patients who have not responded to or cannot tolerate one or more TNF blockers.
Lawyers are currently filing Xeljanz lawsuits on behalf of patients who suffered these side effects after taking this drug.
- Blood Clots and Death
- The boxed warning notes an increased risk of blood clots and death, especially at the 10 mg twice-daily dose used in patients with ulcerative colitis.
- Cancer Risks
- Patients taking Xeljanz may have a higher risk of developing certain cancers, including lymphomas. In particular, doctors observed a higher rate of lymphomas in patients treated with Xeljanz compared to those treated with other medications for rheumatoid arthritis.
- Cardiac Events
- Xeljanz has been associated with an increased risk of serious heart-related events, including heart attack and stroke.
How Does Xeljanz Work?
Xeljanz decreases a substance called cytokines. Cytokines are proteins in the body that help control the immune system. When our bodies have an infection, cytokines increase to help fight the infection. People with RA make more cytokines than necessary, and this leads to inflammation and pain. Xeljanz disrupts cell signals in the Janus kinase (JAK) pathways to reduce the production of new cytokines, according to the manufacturer.
In people with psoriatic arthritis and ulcerative colitis, the drug works the same way to lower inflammation that causes symptoms.
In July 2019, the FDA limited the use of Xeljanz in adults with ulcerative colitis due to safety concerns. The agency had initially approved the drug for the treatment of any adult with moderately to severely active ulcerative colitis. Now the drug is only approved for adults with ulcerative colitis who have an inadequate response or are intolerant to TNF blockers.
Recommended Dosages
Depending on the reason doctors prescribe the drug, it may have different dosage instructions. Patients can take the medicine with or without food.
People may take Xeljanz or Xeljanz XR with or without certain medications called nonbiologic disease-modifying antirheumatic drugs (DMARD) such as methotrexate. But they should not use it with medications called biologic DMARDs or potent immune-suppressing drugs (immunosuppressants) such as azathioprine and cyclosporine.
Patients with severe liver impairment should not use these drugs. Do not take Xeljanz XR for ulcerative colitis.
Rheumatoid Arthritis
Dosage: Xeljanz 5 mg twice daily or Xeljanz XR 11 mg once daily. The recommended dosage for people with moderate and severe kidney impairment or moderate liver impairment is Xeljanz 5 mg once daily.
Psoriatic Arthritis (in combination with nonbiologic DMARDs)
Dosage: Xeljanz 5 mg twice daily or Xeljanz XR 11 mg once daily. The recommended dosage in patients with moderate and severe kidney impairment or moderate liver impairment is Xeljanz 5 mg once daily.
Ulcerative Colitis
Dosage: Xeljanz 10 mg twice daily for at least eight weeks, then 5 mg twice daily. A higher dose of 10 mg twice daily can be continued for a total of 16 weeks, depending on response.
Patients should talk to their doctors about stopping the drug if they’ve taken 10 mg twice daily for 16 weeks and they’re not getting the benefits they thought they would. Patients should use the lowest possible dose to maintain the benefits. People with moderate and severe kidney impairment or moderate liver impairment should use half the dose recommended for people with normal liver and kidney function.
Xeljanz Effectiveness and Interactions
Pfizer studied the effectiveness of Xeljanz in patients who took the drug alone or with another DMARD such as methotrexate. The company conducted six studies of more than 4,200 patients with moderate to severe RA.
In clinical studies, medication reduced RA joint pain in as little as two weeks. Though for some patients, the drug may take three to six months to work.
In the ORAL Solo Study of patients who took Xeljanz without methotrexate, 30% of tofacitinib patients (71 out of 240) experienced a 20% reduction in tender and swollen joints after two weeks. In comparison, 12% of patients in the placebo group (14 out of 119) experienced the same result.
For ulcerative colitis, the drug can reduce rectal bleeding and stool frequency in as little as two weeks and improve the appearance of the intestinal lining within eight weeks, according to Pfizer.
Drug Interactions
Combining Xeljanz and Xeljanz XR with other immune suppressing medicines that treat rheumatoid arthritis, psoriatic arthritis or ulcerative colitis may increase the risk of infection. The drug’s label recommends against taking the medicine in combination with biologic DMARDs or potent immunosuppressants.
- Actemra (tocilizumab)
- Enbrel (etanercept)
- Humira (adalimumab)
- Remicade (infliximab)
- Rituxan (rituximab)
- Orencia (abatacept)
- Kineret (anakinra)
- Cimzia (certolizumab)
- Simponi (golimumab)
- Stelara (ustekinumab)
- Cosentryx (secukinumab)
- Entyvio (vedolizumab)
- Azathioprine
- Cylcosporine
- Other immunosuppressive drugs
Certain medications that affect liver enzymes, such as rifampin and ketoconazole, may interact with Xeljanz. Depending on the medication, Xeljanz may need to be given at a lower dose or may need to be avoided.
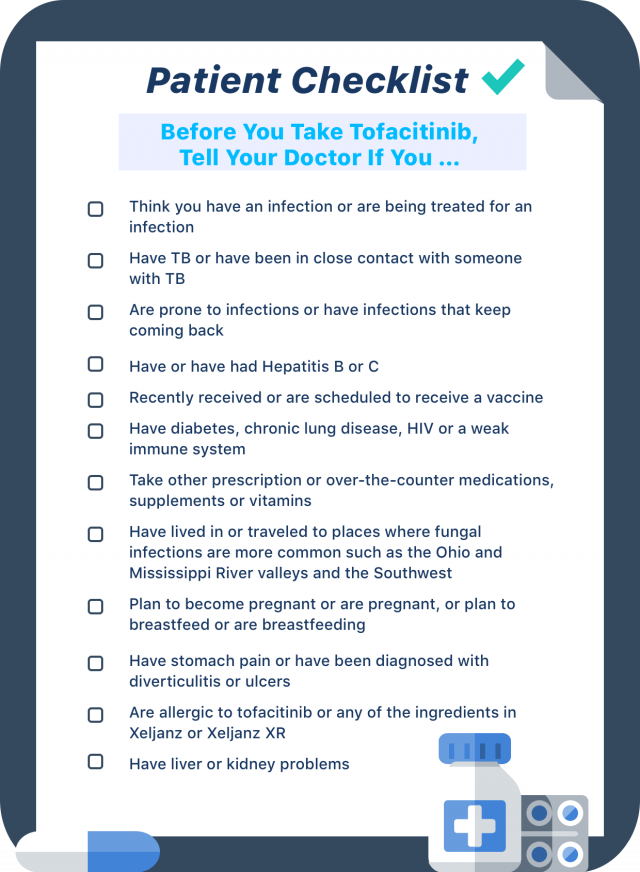
People who plan to take Xeljanz should tell their doctors about all the supplements, vitamins and drugs they take. If this medication is contraindicated for you, discuss possible Xeljanz alternatives with your doctor.
Xeljanz FDA Safety Alerts
Over the years, the FDA has released Xeljanz safety alerts for cancer, serious cardiovascular events and blood clots in the lungs. Other countries such as Australia, Canada and the UK have also added Xeljanz warnings for the same risks.
- December 2021: The FDA approved a boxed warning for serious infections, a higher rate of lymphoma and lung cancers, a higher rate of death, a higher rate of cardiovascular events (stroke, cardiovascular death and heart attack) and blood clots.
- February 2021: The FDA released a safety communication about an increased risk of cancer and serious cardiovascular events in people who took Xeljanz during clinical trials. The most common reported cancer was lung cancer and the most common cardiovascular event was heart attack.
- July 2019: The FDA approved a boxed warning for increased risk of blood clots and death.
- February 2019: The FDA released a safety communication about an increased risk of blood clots in the lungs, known as pulmonary embolisms, and death in patients who took Xeljanz during a safety trial.
When the FDA originally approved Xeljanz, it required Pfizer to conduct a clinical trial to evaluate the risk of heart-related events, cancer and opportunistic infections in rheumatoid arthritis patients who take the drug in combination with methotrexate.
FDA safety monitoring committees found the increased risk of cancer, heart-related events and blood clots after it reviewed the results from the ongoing study as well as additional data. The increased risk occurred specifically in people with rheumatoid arthritis who took 10 mg of the drug twice daily. The FDA has not approved this dose for people with RA but has approved it in patients with ulcerative colitis, and the FDA is concerned that these risks could also occur in people with UC.
In a long-term ulcerative colitis extension study, four people had pulmonary embolisms and one patient with advanced cancer died, according to a Dear Healthcare Provider letter.
The FDA continued its investigation, and on July 26, 2019, the agency approved adding a black box warning about an increased risk of blood clots and death.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.