Allergan
Allergan plc is a global pharmaceutical company. It formed when Allergan Inc. merged with Actavis in 2015. Allergan makes Botox. It is also well-known for its eye care products like Refresh and Restasis. Some of its products such as Viberzi have led patients to file injury lawsuits. In July 2018, the company finalized a settlement to end hundreds of Androderm testosterone lawsuits.
Allergan plc makes pharmaceuticals, medical devices and consumer health care brands. One of Allergan’s most well-known brands is Botox.
Over the years, Allergan has acquired other companies. Some of the companies had made problematic products, such as the Seri surgical scaffold and SSRI antidepressants Celexa and Lexapro. Allergan was acquired by AbbVie Inc. in May 2020 for $63 billion.
Allergan also faces lawsuits over some of its newer drugs, including its antidiarrheal drug, Viberzi.
In July 2018, Allergan finalized a settlement with 500 people who sued over the company’s testosterone replacement therapy, Androderm.
About Allergan
Allergan operates in about 100 countries. It makes many well-known brands including Botox, Linzess, Viberzi, and Lexapro and Celexa.
The company has its headquarters in Dublin, Ireland, but it employs more than 17,000 employees worldwide.
Its employees are in North America, South America, Europe, the Asia Pacific, the Middle East and Africa.
In 2017, Allergan brought in just shy of $16 billion in revenues, according to a February 2018 press release by Allergan. Brent Saunders is the company’s CEO.
Allergan History
Allergan plc got its start as Allergan Pharmaceuticals Inc. in 1950.
Pharmacist Gavin S. Herbert founded Allergan. He created the company’s first drug alongside chemist Stanely Bly.
They called the drug Allergan. It was an antihistamine administered via the nose.
Next, came the eye drops in 1953. Eye care products were the company’s primary focus before it went public in 1970.
-
1980
SmithKline Beckman acquired Allergan Inc.
-
1989
Allergan Inc. separated from SmithKline Beckman. The FDA approved Botox for medical purposes. Allergan acquired the company that manufactured Botox.
-
2002
Allergan Inc. spun-off its ophthalmic surgical and contact lens businesses into Advanced Medical Optics n/k/a Abbott Medical Optics. Botox Cosmetic received FDA approval.
-
2003
Lawsuits targeted Botox (Botulinum toxin) and the media scrutinized the drug.
-
2013
Allergan Inc. acquired MAP Pharmaceuticals. Allergan Inc. sold its obesity intervention business to Apollo Endosurgery.
-
2015
Actavis acquired Allergan Inc. The merged company took the Allergan name as Allergan plc. Allergan and Pfizer attempted a $160 billion merger. It ultimately failed due to new U.S. Treasury rules banning tax inversions in 2016.
-
2016
Teva Pharmaceuticals bought Actavis generics. Allergan acquired eight subsidiaries, including Vitae Pharmaceuticals, RetroSense Therapeutics and Motus Therapeutics.
-
2017
Botox revenues reached $2.2 billion. Allergan acquired LifeCell, Keller Medical and two other companies.
-
2018
Allergan announced its plan to sell its women’s health and infectious disease businesses. It also announced it would settle Androderm lawsuits.
Allergan Products
Allergan products include pharmaceuticals, consumer health care products and medical devices. The company specializes in products for the central nervous system, eye care, aesthetics medicine and gastroenterology.
- Actonel/Actonel DR
- Slows calcium loss from the bones
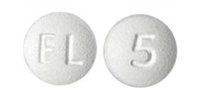
- Androderm
- Testosterone replacement therapy
- Botox
- Neuro-muscular blocker
- Bystolic
- Beta-blocker
- Celexa/Lexapro/
Sarafem - SSRI antidepressants
- Fetzima
- SNRI antidepressant
- Juvederm
- Injectable gel dermal filler for the face
- Kybella
- Injectable synthetic substance that destroys fat cells under the chin
- Latisse
- Treats inadequate or not enough eyelashes
- Liletta
- Hormone-releasing (levonorgestrel) intrauterine device
- Linzess
- Treats bowel/intestinal conditions with constipation
- Loestrin/Taytulla
- Birth control pill/combination norethindrone acetate and ethinyl estradiol and ferrous fumarate (iron supplement to prevent or treat anemia)
- Microzide
- Diuretic
- Namzaric
- Treats dementia caused by Alzheimer’s disease
- Oxytrol
- Treats overactive bladder
- Refresh
- Artificial tears/eye drops
- Restasis
- Treats chronic dry eye caused by inflammation
- Saphris
- Treats bipolar disorder or schizophrenia
- Savella
- Treats fibromyalgia
- Tazorac
- Treats psoriasis or acne in teens and adults
- Teflaro
- Cephalosporin antibiotic that treats skin infections and bacterial pneumonia
- Viberzi
- Treats irritable bowel syndrome with diarrhea
- Xen
- Treats glaucoma
- Zymaxid
- Fluoroquinolone antibiotic that treats bacterial eye infections
Allergan Recall
Allergan has had to recall some of its products. Reasons include improper packaging or similar defects that could lead to patient harm.
-
2013
Product Recalled – Seri Scaffold surgical mesh
Reason for Recall – Outer pouch seal of dual packaging may be compromised and sterility may not be assured -
2015
Products Recalled – Refresh Lacri-Lube, Refresh P.M., FML, Blephamide
Reason for Recall – Potential contamination that could cause eye pain, eye swelling, ocular discomfort or eye irritation -
2018
Product Recalled – Taytulla (birth control pill)
Reason for Recall – Four placebo capsules placed out of order; patients may receive four non-hormonal placebo capsules for the first four days of therapy instead of the active capsules
Allergan Lawsuit
Some of Allergan’s drugs and devices have caused patient injuries that led to lawsuits.
Product liability lawsuits filed against the company allege negligence and fraud. They say the company failed to warn of dangerous risks and promoted the drug for off-label — or unapproved — uses.
Androderm
Patients injured by the testosterone replacement drug Androderm filed lawsuits against Allergan. The drug’s original maker, Actavis, is named in the testosterone lawsuits as well.
Lawsuits say patients suffered from severe and even life-threatening side effects after using Androderm. Testosterone side effects alleged in lawsuits include heart attacks, blood clots and sudden death.
Allergan agreed in 2018 to settle more than 500 cases currently pending in federal court.
Viberzi
Patients who suffered side effects after taking Viberzi are filing lawsuits against Allergan. They claim the antidiarrheal drug led to severe acute pancreatitis.
Some of these patients also suffered from a condition called sphincter of Oddi spasm. The sphincter of Oddi is a muscular valve that regulates the flow of bile and pancreatic juice into the duodenum, a part of the intestine. Two people affected by these conditions have died.

The lawsuits over Viberzi are still in the early stages. No large settlements have been announced.
Celexa and Lexapro
Patients injured by the SSRI antidepressants Lexapro and Celexa sued Forest Laboratories. Actavis acquired Forest Laboratories before merging with Allergan Inc. to create Allergan plc.
Patients who took these medications were at a greater risk for committing suicide. Also, women who took these drugs while pregnant had babies with birth defects.
Thousands of lawsuits over Celexa and Lexapro were pending against the drug manufacturer at the height of litigation.

Forest Laboratories paid millions of dollars in verdicts and settlements. This includes more than $7 million in a class action settlement.
In 2010, Forest Laboratories also pleaded guilty to criminal charges involving the SSRIs.
The U.S. Attorney’s Office in Boston was asked to reopen a criminal case against the drug maker in early 2018. Allegations involve the misrepresentation of the drugs’ safety.
Seri Surgical Scaffold
Patients implanted with Seri surgical scaffold sued Allergan after they experienced complications.
Complications of Seri surgical scaffold include tissue death, seromas, hematomas, implant loss, capsular contracture and breast infection.
In mid-2015, the FDA warned Allergan about its marketing of the silk-based surgical mesh. The company marketed the device for breast surgery, despite not having FDA approval for the use.
In 2018, Allergan reached a settlement for an undisclosed amount with a woman who accused the company of promoting the device for breast reconstruction surgery. She suffered disfigurement and required more surgeries.
Allergan acquired the Seri Scaffold technology when it purchased its original maker Serica in 2010. In 2016, Sofregen Medical purchased the product line from Allergan.
Botox
Patients injured after using Botox sued Allergan. They said the drug caused droopy eyelids, numbness, headaches, problems swallowing and breathing, brain damage, and death.
In 2010, Allergan agreed to pay $600 million to the federal government to resolve allegations of off-label promotion of the drug, according to the U.S. Department of Justice.
Jurors ordered Allergan to pay $212 million to a Virginia man who suffered brain damage after using the drug to treat hand tremors — an off-label use. It was the largest penalty ever in a Botox injury case, The Los Angeles Times reported.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


