Truvada Side Effects
The most common side effects of Truvada include rash, headaches, nausea, weight loss and vomiting. Rare but serious side effects include kidney and liver problems, bone loss, potentially fatal lactic acidosis and immune reconstitution syndrome.
Article Continues Below
Board-certified physicians medically review Drugwatch.com content to ensure its accuracy and quality.
Drugwatch.com partners with Physicians’ Review Network Inc. to enlist specialists. PRN is a nationally recognized leader in providing independent medical reviews.
Reviewer specialties include internal medicine, gastroenterology, oncology, orthopedic surgery and psychiatry.
Drugwatch.com has been empowering patients for more than a decade
Drugwatch.com has provided reliable, trusted information about medications, medical devices and general health since 2008. We’ve also connected thousands of people injured by drugs and medical devices with top-ranked national law firms to take action against negligent corporations.
Our team includes experienced medical writers, award-winning journalists, researchers and certified medical and legal experts. Drugwatch.com is HONCode (Health On the Net Foundation) certified. This means the high-quality information we provide comes from credible sources, such as peer-reviewed medical journals and expert interviews.
The information on Drugwatch.com has been medically and legally reviewed by more than 30 expert contributors, including doctors, pharmacists, lawyers, patient advocates and other health care professionals. Our writers are members of professional associations, including American Medical Writers Association, American Bar Association, The Alliance of Professional Health Advocates and International Society for Medical Publication Professionals.
About Drugwatch.com
- Assisting patients and their families since 2008.
- Helped more than 12,000 people find legal help.
- A+ rating from the Better Business Bureau.
- 5-star reviewed medical and legal information site.
Testimonials
"Drugwatch opened my eyes to the realities of big pharmacy. Having a family member with major depression and anxiety, I was looking for information on her medications. I found information that was very helpful, that her psychiatrist never told her."
- Common Side Effects
- Depression, diarrhea, headache, nausea, rash, dizziness, insomnia, abnormal dreams, rash, abdominal pain, weight loss and fatigue.
- Serious Side Effects
- Kidney and liver problems, bone density loss, lactic acidosis and immune reconstitution syndrome.
- Black Box Warning
- Post-treatment acute exacerbation of hepatitis B and risk of drug resistance with use of Truvada for HIV-1 pre-exposure prophylaxis, or PrEP, in undiagnosed early HIV-1 infection.
Latest Side Effects Information for Truvada
According to the U.S. Food and Drug Administration’s Adverse Event Reporting System, or FAERS, there have been over 35,000 adverse event reports for Truvada from 2005 to Mar. 31, 2024.
| FDA Adverse Events Reporting System (FAERS) Data for Truvada Side Effects | |
|---|---|
| Total cases reported | 35,263 |
| Serious cases (including deaths) | 35,263 |
| Deaths | 1,222 |
Disclaimer: Reports sent to the FDA don’t necessarily mean the drug caused an adverse event. Consult a health care professional before stopping or changing medication.
Truvada has a black box warning that explains that symptoms of Hepatitis B (HBV) may worsen in patients who stop taking the drug. Patients who discontinue Truvada or other drugs containing Tenofovir Disoproxil Fumarate (TDF), one of Truvada’s active ingredients, may have severe flare-ups of HBV symptoms. In these situations, the patient may need to restart hepatitis therapy.
Truvada also has a black box warning stating that only patients who are negative for human immunodeficiency virus (HIV) should use the drug for Pre-Exposure Prophylaxis (PrEP) purposes. PrEPs are used to help prevent HIV infection.
The most common side effects are temporary and mild, lasting a month or less. The most serious long-term side effects of Truvada are kidney and liver problems and bone loss.
People who experienced these serious side effects filed lawsuits against Gilead Sciences, Inc., the manufacturer of Truvada. Court documents say the drug maker failed to warn the public of these risks properly.
Common Emtricitabine/Tenofovir Side Effects
Common side effects related to Truvada may vary depending on HIV infection, HBV infection and kidney health, according to the medication insert.
- Abdominal pain
- Back pain
- Depression
- Diarrhea
- Dizziness
- Fatigue
- Headache
- Insomnia
- Itching or skin rash
- Joint pain
- Nausea
- Sinusitis
- Skin discoloration and hyperpigmentation
- Stomach pain
- Strange dreams
- Trouble sleeping
- Upper respiratory tract infection
- Vomiting
- Weight loss
Pediatric patients experienced the same side effects as adults.
Experts recommend regular monitoring of kidney and liver function and bone density to avoid long-term side effects.
Pediatric patients experienced the same side effects as adults.
Most short-term side effects at the beginning of treatment involve gastrointestinal symptoms, according to a 2017 study published in the Official Journal of the International Society of Pharmacovigilance. The same study found that the side effects typically resolve within a month.
Experts recommend regular monitoring of kidney and liver function and bone density to avoid long-term side effects.
Additionally, no clinical trials or post-marketing reports have linked Truvada to hair loss. If you experience this side effect while taking this drug, consider informing your health care provider.
Serious Side Effects of Truvada
In rare instances, Truvada can lead to significant kidney issues, which can worsen kidney damage and cause bone problems.
- Kidney damage and other problems
- Bone density loss
- Immune reconstitution syndrome
- Lactic acidosis
Studies link Truvada’s ingredients to these side effects. There are specific symptoms to look out for when monitoring your kidney function.
Kidney Problems
Truvada’s label has warnings for new onset or worsening kidney impairment. Kidney impairment can include acute renal failure and Fanconi syndrome.
Fanconi syndrome is a rare condition affecting kidney tubules’ function, which impacts the kidney’s ability to reabsorb certain substances. As a result, patients with Fanconi syndrome excrete an overabundance of glucose, bicarbonate, phosphates, uric acid, potassium and certain amino acids through their urine. Too much depletion of these substances can lead to worsening kidney damage and bone problems.
Before patients begin Truvada treatment, health care providers should test kidney function.
- Fractures
- Pain in extremities
- Persistent bone pain
- Muscular pain or weakness
Several studies link Tenofovir Disoproxil Fumarate (TDF), one of the active ingredients in Truvada, to kidney problems.
Clinical trial data reassured doctors that TDF would not have the same kidney toxicity as other drugs in its class. Yet, in a 2013 article published in the Journal of the American Society of Nephrology, Dr. Jérôme Tourret and colleagues highlighted the publication of the first case of TDF-induced acute nephrotoxicity in 2001.
“Numerous cases have been published since then, and it is now established that TDF presents a tubular toxicity risk,” the study authors wrote.
“[I]t is now established that TDF presents a tubular toxicity risk.”
According to Truvada’s label, some HIV-infected patients who started high-dose or multiple NSAIDs reported acute renal failure. Some patients ended up hospitalized and on renal replacement therapy.
A July 2022 study published in BioMed Central’s Journal of Infectious Diseases looked at the kidney safety of Truvada during pregnancy. Researchers didn’t observe any safety concerns for kidney function for the pregnant person or fetus.
Bone Density Loss
Generally, osteopenia and osteoporosis occur in 40 to 90 percent of HIV-infected people. People with HIV also have a 60 percent increased fracture risk compared to uninfected people. Truvada for PrEP or HIV treatment may increase the risk of bone mineral density loss.
According to Truvada’s drug label, cases of osteomalacia, which involves weakened bone linked to kidney damage, may manifest as bone pain or pain in the extremities.
Researchers noted signs of increased bone turnover, which is the rate of bone reabsorption in the body. An increased rate of bone turnover can increase the risk of fracture.
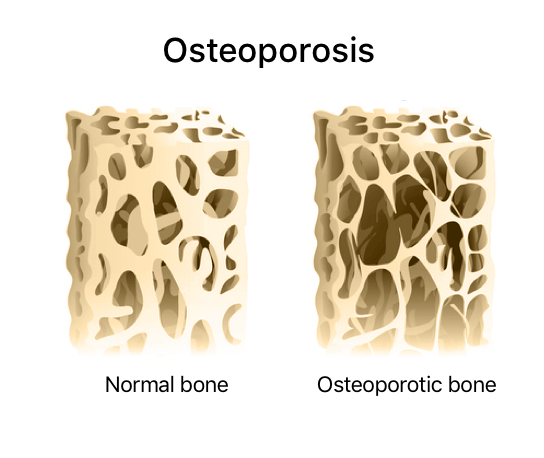
There is mixed evidence on how bone loss from TDF compares to the active ingredients in similar drugs. A 2016 study in the journal Current Opinion in HIV and AIDS found a one to three percent greater bone mineral density loss amongst adults taking TDF compared to other HIV drugs.
However, a small 2017 study in the International Journal of Antimicrobial Agents that followed 26 HIV-infected youths for ten years, found that TDF-containing drugs did not impair bone mineral density in young patients.
“Larger studies are needed to confirm these results,” authors V. Giacomet and colleagues wrote.
Immune Reconstitution Syndrome
Immune reconstitution syndrome — also called immune reconstitution inflammatory syndrome, or IRIS, is a collection of disorders that occurs when preexisting infections worsen after starting highly active antiretroviral therapy drugs such as Truvada.
This condition can occur in about 10 to 40 percent of HIV patients with low CD4+ T-cell counts. A T-cell is a white blood cell that helps the immune system. A T-cell count of less than 50/μL and a high amount of HIV in the blood are the most common risk factors for IRIS, according to an article published in The Medical Journal of Australia.
Patients with IRIS may develop symptoms anywhere from one week to a few months after starting therapy.
During the initial phase of TDF therapy, patients may experience infections that require treatment, such as pneumonia, cytomegalovirus, Mycobacterium avium infection or tuberculosis.
In addition, autoimmune disorders such as Graves’ disease, Guillain-Barre and polymyositis have occurred in patients.
Lactic Acidosis
Though rare, some patients who used Truvada alone or in combination with other antiretrovirals have experienced lactic acidosis — a buildup of acid in the blood — and severe hepatomegaly with steatosis, which involves an enlarged liver. Some of these were fatal.
In one case reported in the National Journal of Medical Research, a 50-year-old man with HIV switched to tenofovir, lamivudine and efavirenz. After three days on this combination, he experienced nausea, vomiting, upper abdominal pain and breathlessness.
Doctors diagnosed him with lactic acidosis and hepatitis induced by tenofovir. He improved after he stopped taking tenofovir.
It can also affect people with HBV. In a case published in the journal Medicine, a 59-year-old man with HBV developed lactic acidosis after ten days on TDF. Despite stopping TDF and starting hemodialysis, the patient died.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


