Legal and Health Risks Facing Older Adults
Older adults might experience serious side effects from prescription drugs, medical devices or long-term exposure to toxins. Health issues caused by some products have led to lawsuits. Talk to your doctor or a lawyer if a potentially harmful product has injured you or a loved one.
Some products used by older adults, like hip replacements, Type 2 diabetes medications and weed killers, are linked to major health risks. Side effects may include chronic pain, digestive issues and an increased cancer risk.
These complications have caused older adults and their families to file lawsuits against some product manufacturers. Senior health lawsuits claim companies that manufactured defective products failed to warn the public about possible health risks.
Hip Replacement Complications and Lawsuits
People suffering from hip replacement complications have filed lawsuits against certain manufacturers. Hip replacement lawsuits argue that poor device design causes corrosion and fretting when metal components rub together and wear down.
Corrosion or fretting can release metal debris into the body and cause metallosis. This is an inflammatory condition that occurs when metal ions build up in the blood and tissue.
Hip replacement surgery is more common in older adults because of conditions like arthritis and osteoporosis. These expose seniors to health risks from implant complications.
- Elevated metal levels in the blood
- Hip replacement instability
- Metal toxicity (symptoms may include cognitive dysfunction, fatigue, impaired hearing or vision, vertigo and more)
- Pain
- Potential revision surgery
- Tissue damage
Major manufacturers involved in past and current hip replacement lawsuits include Exactech, DePuy, Smith & Nephew, Stryker and Wright Medical.
Some of these companies issued hip replacement recalls for their devices. For example, in 2023, Exactech issued a recall because of defective packaging that could lead to early device wear and failure.
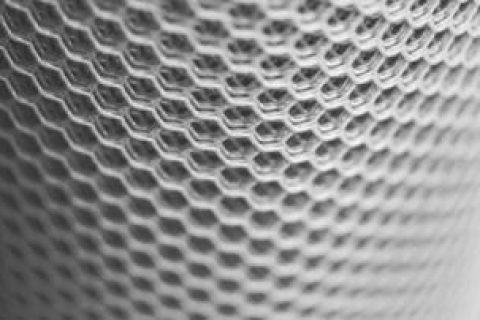
Hernia Mesh Lawsuits
Hernia mesh lawsuits claim that defective hernia meshes can cause complications like chronic pain, hernia recurrence, infection, nerve damage and more.
Older adults, especially men, are at greater risk for hernias because muscles weaken with age. Doctors often use mesh to repair hernias surgically.
C.R. Bard faces the most hernia mesh lawsuits as of May 2025, with 24,078 pending cases. Other manufacturers facing hernia mesh lawsuits include Covidien and Ethicon.
The trial in the case of Patterson v. Covidien is scheduled to begin in February 2026.
IVC Filter Injuries
Inferior vena cava (IVC) filter injuries may include allergic reactions, excess bleeding, infections, leg swelling and organ damage.
Doctors implant IVC filters in a large vein in the abdomen (vena cava) to prevent blood clots from traveling to the lungs. Older adults, particularly men, are more likely to receive IVC filters, putting them at higher risk for IVC complications.
IVC filter lawsuits claim device defects caused some people to suffer injuries or death. One manufacturer, Bard, has already settled thousands of cases. Another manufacturer, Cook Medical, still faces nearly 7,000 lawsuits as of May 2025.
Lawyers are still accepting claims.
Bard PowerPort Complications
The Bard PowerPort is an implantable device that provides a long-term access point for IV medications like chemotherapy. However, lawsuits say that when it breaks, it can cause complications, including infections, organ punctures and blood clots.
Cancer risk increases with age, making older patients more likely to need an implantable port for medications. Research on implantable ports published in JCO Oncology Practice found that most patients in the study had an average age of 66.
Becton Dickinson and its subsidiaries, C.R. Bard and Bard Access Systems, manufacture these devices. They are the defendants in PowerPort lawsuits.
Plaintiffs allege the PowerPort’s design is defective and may cause it to break, leading to serious health risks. Lawsuits also claim manufacturers never warned the public of the PowerPort’s high failure rate.
Impella Heart Pump Injuries
Impella heart pump lawsuits claim the devices have design defects that could lead to failure, causing potentially fatal complications.
Doctors may use the Impella heart pump during catheter-based cardiac procedures, open-heart surgery or if your heart isn’t functioning well.
- In June 2023, the recall was for damaged motor blades that may cause reduced blood flow or stop the pump from working.
- In December 2023, the agency announced the recall of over 66,000 devices because the pump catheter could cut into the heart’s left ventricle wall.
In the recall announcements, the FDA warned that complications of malfunctioning Impella heart pumps could be life-threatening in patients needing high levels of heart support or if the broken blade pieces get into the patient’s bloodstream.
Valsartan and Cancer Risk
In 2018, the FDA issued a voluntary recall of medications containing valsartan. The recall was due to potential contamination with N-nitrosodimethylamine (NDMA), a substance that might be carcinogenic.
Valsartan is a prescription medication for high blood pressure. More seniors may have been exposed to valsartan than other age groups, as 70% of adults aged 65 or older have high blood pressure.
Many people who were diagnosed with cancer after taking valsartan have filed lawsuits. Some of the cancers mentioned in valsartan lawsuits include intestinal, liver cancer, prostate and stomach.
As of May 2025, over 1,300 lawsuits are pending in New Jersey.
Taxotere and Permanent Hair Loss
Taxotere (docetaxel) is a chemotherapy drug that treats a variety of cancers. Studies have linked it to permanent hair loss.
According to research published in Breast Cancer Research and Treatment, about 10% of Taxotere users had to wear a wig after treatment because of permanent hair loss.
A common side effect of chemotherapy is hair loss. However, Taxotere lawsuits say the manufacturer didn’t warn them that the chemotherapy drug could cause permanent hair loss from destruction of hair follicles.
Since 60% of cancer patients are 65 or older, older adults might be more likely to be exposed to docetaxel for chemotherapy treatments.
Taxotere Eye Injuries
Another group of Taxotere lawsuits alleges eye injuries from docetaxel. The plaintiffs claim they suffered permanent damage to their nasolacrimal drainage systems, impacting tear production. This damage resulted in excessive tears that led to swollen, watery eyes.
Camp Lejeune Water Contamination
Many older veterans and their families could be affected by the U.S. Marine Corps Base Camp Lejeune water contamination from the 1950s to the 1980s. The contamination resulted from leaks in underground fuel storage tanks.
Chemicals that contaminated the water supply included benzene, trichloroethylene (TCE) and perchloroethylene (PCE). According to the U.S. Department of Veterans Affairs, these chemicals are associated with several types of cancer, female infertility, miscarriage, Parkinson’s disease and other conditions.
Camp Lejeune Justice Act of 2022
The Honoring our Promise to Address Comprehensive Toxics (PACT) Act of 2022 includes the Camp Lejeune Justice Act (CLJA) of 2022. This legislation allowed veterans to file a claim for injuries caused by Camp Lejeune water contamination.
The Navy’s filing deadline passed in August 2024, but some lawyers are still accepting Camp Lejeune lawsuits.
Paraquat and Parkinson’s Disease
Studies have shown that Parkinson’s is more likely to occur in patients exposed to paraquat for longer durations. Research in the International Journal of Epidemiology also found that people who live and work near agricultural facilities using higher amounts of paraquat have a greater risk of developing Parkinson’s.
Seniors already have higher odds of developing Parkinson’s, so exposure to paraquat could increase their risk.
Scientists are still researching how paraquat increases Parkinson’s risk. A study in Environmental International proposed that paraquat may lead to Parkinson’s by causing inflammation in the midbrain, which is associated with motor control.
Paraquat Lawsuits Close to Settlement
Thousands of paraquat lawsuits claim the herbicide led people to develop Parkinson’s.
In one paraquat lawsuit, plaintiff Paul Friday said he used paraquat on a peach farm from 1962 through 2013 before developing Parkinson’s. He claims he couldn’t have known that paraquat was connected to Parkinson’s disease because Syngenta withheld the information.
In April 2025, paraquat’s maker, Syngenta, moved to settle these cases. The final details haven’t been released.
PFAS and Cancer in Seniors
Research shows exposure to PFAS (per- and polyfluoroalkyl substances) may increase the risk of developing certain cancers. The strongest evidence links PFAS to kidney, prostate and testicular cancer.
One study in the Journal of the National Cancer Institute found people with the highest levels of PFOA (a type of PFAS) in their blood had a more than two-fold increase in a common form of kidney cancer called renal cell carcinoma.
PFAS are chemicals used in the manufacturing of several products. They may be found in grease-resistant food packaging, firefighter turnout gear, nonstick cookware and waterproof clothing.
These chemicals break down slowly and remain in your body for a long time, leading to a buildup. Older adults have higher levels of PFAS in their blood, increasing their risk of developing cancer.
PFAS Lawsuits
PFAS water contamination lawsuits allege that chemical companies like 3M and DuPont are responsible for contaminating water with PFAS, leading to cancer and other health problems.
Aqueous film-forming foam (AFFF) lawsuits claim that firefighting foam made with PFAS endangers firefighters and increases their cancer risk.
Suboxone Tooth Decay Lawsuits
Suboxone tooth decay lawsuits claim the drug’s maker, Indivior, didn’t disclose the risk of cavities, oral infections, tooth decay and tooth loss caused by the drug’s sublingual film version. Lawsuits say Indivior made Suboxone acidic, leading to dental issues.
Doctors prescribe Suboxone to treat opioid dependence. Chronic pain increases with age, putting older adults at increased risk of potential opioid dependence that may require medication like Suboxone to treat.
Roundup and Cancer in Retired Workers
Retirees who worked in farming, landscaping or groundskeeping may have been exposed to Roundup (glyphosate) weedkiller for decades. Studies have linked Roundup to an increased risk of non-Hodgkin lymphoma.
Roundup lawsuits claim that Monsanto, Roundup’s maker and a subsidiary of Bayer, didn’t warn the public about the product’s cancer risk. A lawsuit filed by John Barnes in 2021 claims Monsanto covered up the risk. In March 2025, a jury awarded Barnes $2.1 billion in damages.
Bayer set aside about $10 billion in 2020 to settle roughly 125,000 Roundup lawsuits. Lawyers are still accepting cases.
Ozempic and GLP-1 Drug Complications
Ozempic belongs to a drug class that treats type 2 diabetes called GLP-1, but is often used off-label for weight loss. According to Ozempic lawsuits, these medications may lead to complications like stomach paralysis (gastroparesis), intestinal obstruction and other gastrointestinal injuries.
Lawsuits against Ozempic and other GLP-1 manufacturers also allege that drug makers failed to warn users about the risk of gastrointestinal problems and made inaccurate claims about the medication’s safety.
GLP-1 drugs like Ozempic treat type 2 diabetes, a condition occurring more often in middle-aged and older adults. Consequently, seniors may be at increased risk of complications from these medications since they are more likely to need them.
What Seniors (or Their Families) Should Do If Harmed
Older adults who were harmed by a drug, medical device or toxic substance should talk to their doctor about treatment options. Speaking to a lawyer immediately is also important if you want to file a lawsuit. They’ll want to track your use of the drug or device, symptoms and collect other documentation.
Keep Medical and Product Documentation
Keep copies of all your medical documents, including dental records, X-rays, doctor’s notes and prescriptions. Holding onto product packaging can also be helpful.
This information is crucial for getting the best treatment. It can also help prove you were exposed to a particular product if you want to file a lawsuit.
Seniors may need help from caregivers or family members to gather information.
Consult a Doctor and Product Liability Lawyer
Consulting a doctor for treatment options or a prognosis is critical, especially for life-threatening diseases like cancer. A doctor may also be able to connect your illness to a specific product.
If you want to file a lawsuit, you should speak with a lawyer. A product liability lawyer can help you determine if you have a case.
Contacting a lawyer immediately is important because you may have a limited time to file a case, which is called the statute of limitations. This varies from state to state, but missing that window could prevent you from filing a claim.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.