Warfarin
Warfarin (brand name Coumadin) is one of the original anticoagulant medications, also referred to as blood thinners. It is used to prevent and treat blood clots and to prevent strokes from atrial fibrillation. Warfarin requires regular blood testing and frequent dosage adjustments. It is also linked to increased bleeding risks, which can sometimes be fatal.
Warfarin (Coumadin) is an anticoagulant (blood thinner) that has been on the U.S. market for over six decades since its initial approval by the U.S. Food and Drug Administration in 1954.
This drug has a black box warning for serious bleeding. Patients taking warfarin must get frequent lab work measuring the International Normalized Ratio (INR), a blood-clotting measurement.
The test helps determine dosage. Changes to diet, starting or stopping other drugs, and certain lifestyle choices, such as alcohol intake or cigarette smoking, can alter a patient’s INR.
What Does Warfarin Treat?
Warfarin prevents and treats clots from forming in the blood. The drug prevents problems due to certain types of irregular heartbeats. It is also used in patients who have suffered a heart attack or have prosthetic heart valves.
Warfarin is used to prevent and treat venous thrombosis (a blood clot in a vein), as well as a related condition, pulmonary embolism. A pulmonary embolism happens when part of a blood clot breaks away and becomes lodged in an artery supplying blood to the lungs.
Warfarin is also used to prevent and treat strokes associated with atrial fibrillation (AF or AFib). AF is the most common heart-rhythm abnormality, according to the FDA.
The condition is characterized by an irregular and often rapid heart rate that can increase a patient’s risk of suffering from stroke among other serious and sometimes deadly conditions, such as heart failure and other heart-related complications.
Warfarin may also be prescribed to reduce the risk of death from heart attacks and thromboembolic events, such as stroke or systemic embolization (a blocked artery often caused by a blood clot) after a heart attack.
Warfarin’s Black Box Warning: Bleeding Risk
Warfarin contains a black box warning for major and life-threatening bleeding risks. Since the drug is designed to prevent blood from clotting, it can also take longer than usual for patients to stop bleeding if they are cut or injured.
Bleeding linked to warfarin use can also result in increased menstrual flow or vaginal bleeding in women, nosebleeds and bleeding of the gums from teeth brushing.
As of 2022, the drug label advises patients to report any unusual bleeding, bruising or other signs and symptoms of internal bleeding, such as headache, dizziness or weakness to their health care provider.
Additionally, health care providers should perform regular monitoring of INR levels for patients treated with warfarin. If the INR level is too high, there is an increased risk of bleeding.
Warfarin Side Effects?
Aside from bleeding, warfarin use is associated with several other side effects. These side effects can range from mild adverse reactions, such as nausea or abdominal pain, to rare but serious complications, such as calciphylaxis (calcium build-up in small blood vessels of the fat and skin tissues) and tissue necrosis (death of body tissue).
Serious side effects of Warfarin
- Hemorrhage (severe bleeding)
- Tissue necrosis or gangrene (death of skin or body tissues)
- Calciphylaxis (calcification of blood vessels) – this condition can lead to blood clots and skin necrosis
- Acute kidney injury
- Cholesterol embolism (blockage of an artery, typically by a clot) – this condition occurs when cholesterol is released, usually from plaque build-up in the arteries, and travels through the bloodstream becoming lodged in blood vessels in various parts of the body
- Decreased blood flow to limbs, tissue death and gangrene in patients with heparin-induced thrombocytopenia (low blood platelet count) (HIT) and HITTS (heparin-induced thrombotic thrombocytopenia syndrome)
The most common side effects reported in patients taking Coumadin include:
- Hypersensitivity or allergic reaction – can result in hives as well as anaphylaxis. Anaphylaxis requires immediate emergency medical attention
- Inflammation of the skin (dermatitis), including bullous eruptions (fluid-filled blisters)
- Elevated liver enzymes
- Nausea and/or vomiting
- Diarrhea
- Changes in the sense of taste
- Abdominal pain
- Hepatitis (inflammation of the liver) – cholestatic hepatitis has also been found to occur in patients taking both warfarin and ticlopidine (a drug that also helps to prevent blood clots) together
- Vasculitis (inflammation and damage to blood vessels, primarily in the skin)
- Gas and/or bloating
- Rash
- Itchy skin
- Hair loss
- Feeling cold or chills
How Does Warfarin Work?
The drug works by slowing down the blood-clotting process. Clots form through a process involving various substances, including vitamin K. The drug decreases the amount of vitamin K in the body. The decrease in vitamin K prolongs the time it takes to form clots, which can decrease new clots from forming.
The drug does not dissolve or break down blood clots. However, by slowing down the time for blood to clot, warfarin can help treat an existing clot by stopping the clot from spreading. It also gives the body time to break down the clot on its own.
Blood Tests, Vitamin K

The Prothrombin Time (PT) is a laboratory test showing the time it takes blood to clot. The PT is reported as a value known as the International Normalized Ratio (INR). When patients are prescribed warfarin, they are required to undergo regular testing to make sure the INR measurement stays within the desired testing range. Testing occurs at least once a month but may be more frequent. If the INR is too high, bleeding may occur. If the INR is too low, blood clots may form. Warfarin dosing is based on INR values.
Vitamin K intake can affect the INR/PT measurement as well as the effectiveness of the drug. The American Heart Association states that patients should keep vitamin K intake “as consistent as possible.” Sudden increases of vitamin K foods may decrease the INR and warfarin’s effect, which could cause blood clots. While lowering vitamin K intake can increase INR and the effect of the medication.
One way to keep vitamin K intake consistent is to not make too many dietary changes, or modifications in food choices, and to carefully consider any dietary supplements or herbal products. Since dosing is dependent on each patient’s INR measurements, patients should not entirely stop eating vitamin K-rich foods that they normally eat, nor should they suddenly add foods or supplements rich in vitamin K to their normal daily diets. Changes in diet should be reported to a healthcare provider.
- Kale
- Spinach
- Collards
- Swiss chard
- Mustard greens
- Turnip greens
- Parsley
- Broccoli
- Brussels sprouts
- Cabbage
- Green leaf lettuce
- Romaine lettuce
- Prunes
- Asparagus
- Avocado
- Endive
- Tuna
- Blueberries
- Blackberries
- Peas
Administration and Dosages
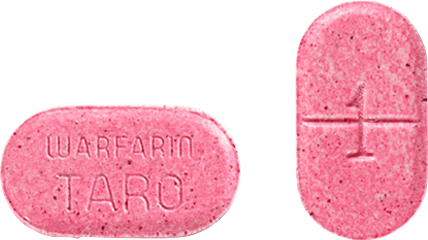
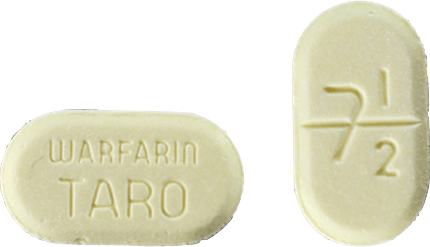
Warfarin comes in a tablet form to be taken by mouth. The tablets are available in several different strengths. Health care providers will likely start patients on a lower dose and gradually increase or decrease the dose based on results of INR blood tests. Drug labeling for warfarin advises patients not to stop taking the medication without first talking to their doctor.
Tablet Strengths and Descriptions







Warfarin’s Dosage and Duration
The dosage and administration of warfarin is individualized for each patient according to their blood tests and conditions.
Lower initial doses are recommended for patients who are elderly, weakened or of Asian descent. Duration of treatment will also vary from one patient to the next with therapy generally being continued until the risk of blood clotting has passed.
Certain dental or surgical procedures may require a temporary interruption or change in warfarin treatment due to bleeding risks.
Overdosage of Warfarin (Coumadin)
The primary concern with overdosage in patients taking warfarin is the risk for bleeding. Taking too much of the anticoagulant can result in several signs and symptoms that a dose adjustment is needed. Many of these symptoms can signal life-threatening bleeding and require immediate medical intervention.
Signs and symptoms of Coumadin overdose may include:
- Excessive bruising or persistent oozing from superficial injuries (any injury that does not affect underlying muscles or organs, typically only affecting the skin)
- Blood in the stool or urine
- Excessive menstrual bleeding in women
- Unexplained fall in hemoglobin (a lab value that may indicate blood loss)
- Dark, sticky stool containing blood
- Pinpoint, round spots that appear on the skin
- Blood in vomit
Treatment of overdose is based on the patient’s INR level, the presence or absence of bleeding and other clinical circumstances. Reversal of the medication’s effects may be achieved by discontinuing the drug and administering vitamin K.
Warfarin Drug Interactions
Certain drugs, and even herbal or dietary supplements, can interact with warfarin. Additionally, more frequent blood monitoring is needed when a patient starts or stops other drugs, including supplements, or when dosages of other drugs are changed.
Enzyme Inhibitors and Inducers
Certain drugs, such as those belonging to the class of inhibitors of CYP2C9, 1A2 and/or 3A4 (certain enzymes found in the body), have the ability to increase the effect of warfarin. These medications include certain antifungals, decongestants, Xanax (alprazolam) and caffeine. Other substances that induce these enzymes may have the opposite effect on warfarin. These include certain anti-seizure drugs and cigarettes.
Drugs That Increase the Risk of Bleeding
These can include certain pain medications, such as aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, serotonin reuptake inhibitors (SRIs) used to treat depression and anxiety disorders, and use of other medications that can thin the blood (antiplatelets and other anticoagulants).
Herbal and Dietary Supplements
Many dietary supplements and herbal medications interact with warfarin and alter a patient’s INR/PT levels. This may increase or decrease the effect of warfarin.
- Co-enzyme Q10
- Echinacea
- Garlic
- Ginkgo biloba
- Ginseng
- Goldenseal
- St. John’s Wort
- Any vitamin/mineral supplements that list vitamin K on the label
Antibiotics and Antifungals
Some antibiotics can interfere with the effect of warfarin. There have been reports of changes in INR in patients taking warfarin and certain antibiotics or antifungals, according to drug labeling for warfarin.
Alcoholic Beverages
Alcohol can affect dosing of warfarin. It is best to limit alcohol while taking warfarin and avoid drinking it on a daily basis.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


