Pregnancy
Pregnancy occurs when a man’s sperm fertilizes a woman’s egg. It travels through the fallopian tube and implants itself in the uterine wall. Pregnancy usually lasts about 40 weeks divided into three trimesters. Many women experience uncomfortable symptoms and physical changes during pregnancy. To decrease the risk of complications, women should practice proper prenatal care, avoid dangerous drugs and choose the best method of delivery for them.
A woman usually knows she is pregnant when she misses one or more periods. However, missing a period does not always mean a woman is pregnant, and women often experience other symptoms of pregnancy before missing a period. While some women experience multiple symptoms, others don’t experience any.
- Nausea and vomiting (morning sickness)
- Slight bleeding
- Swollen breasts or nipples
- Fatigue
- Headaches
- Mood swings
- Food cravings
- Frequent urination
These symptoms are also similar to those of premenstrual syndrome (PMS) and other medical conditions. To confirm pregnancy and rule out other medical conditions, women should talk to their doctors if they notice any of these signs.
Many women use a home pregnancy test before calling their doctor. The tests do not require a prescription and are typically accurate. The best time to take the test is a week after the first missed period or at least one to two weeks after sex.
- Pregnancies last three trimesters, for a total of roughly 40 weeks.
- Common side effects of pregnancy include nausea, vomiting, swelling, varicose veins, backaches, hemorrhoids, heartburn, fatigue, constipation and sleep loss.
- Proper prenatal care and avoidance of harmful substances and drugs can increase the chances of a healthy pregnancy.
- Pregnancy complications can occur from improper prenatal care and preexisting conditions, or for no obvious reason at all. But most complications are treatable if detected early.
- The variety of methods for giving birth range from natural births to C-sections and water births to deliveries in a hospital bed.
- Women should maintain open communication and regular contact with their healthcare providers throughout their pregnancies.
First Trimester
The first trimester lasts 12 weeks, beginning with conception. During this trimester, substances such as alcohol, illicit drugs, certain medicines and illnesses can do the most damage to the fetus. According to the American College of Obstetricians and Gynecologists, this trimester is also the riskiest for miscarriages, with approximately 80 percent occurring in the first trimester.
After eight weeks, the embryo becomes a fetus and is one inch to an inch and a half long. By week 12, the fetus begins to move more frequently, and its genitals are developed. Eyelids, toenails and fingernails appear.
From week one through four, women usually experience symptoms such as breast tenderness, mood swings, constipation, bloating and heightened senses — such as taste and smell. Morning sickness begins around week six for some women. This may last until the second trimester.
Weeks seven and eight bring symptoms such as frequent urination, headaches and extra saliva. Reduced blow flow may cause some women to have dizzy spells throughout the day.
First Doctor’s Visit
Women should schedule their first doctor’s visit sometime during weeks six through eight or after their menstrual period is two to four weeks late. Some doctors will not schedule the first exam until week eight unless there is an issue.
During the first visit, the doctor will ask many questions about the woman’s health, habits and menstrual cycle. The doctor will also perform a number of tests or exams. Women of different ethnic backgrounds often take different tests because they may be at a higher risk for certain diseases.
- A physical
- A pelvic and rectal exam
- A complete blood cell count
- A urine sample
- A pap test
- Blood typing and screening
- A test for infections such as syphilis, hepatitis, gonorrhea, chlamydia and HIV
- A test for previous exposure to chickenpox, measles or mumps
- A test for cystic fibrosis
Exam Timeline
If the initial exam does not produce warning signs women generally see the doctor on a set schedule. Between the 10th and 14th weeks, women may be screened for substances that could point to risk factors for later complications. Between 24 and 28 weeks, pregnant women are tested for gestational diabetes, a type of diabetes that forms during pregnancy. Women who are at higher risk for gestational diabetes may be tested sooner.
- Every four weeks until the 28th week
- Every two weeks from weeks 28-36
- Once a week from week 36 to delivery
Second Trimester
The second trimester lasts from week 13 to week 28.
As early as week 12, but usually around week 16, a doctor can determine the sex of the fetus. Bones, muscle tissue and skin have formed by then.
Women usually feel movement around the 20th week. Around the 24th week, footprints and fingerprints are formed and the fetus sleeps and wakes frequently. The size and shape of the woman’s uterus may also be measured in the 22nd week to determine whether the fetus is growing and developing normally.
The 28th week is usually the earliest a baby can be born, with an estimated 92 percent of babies surviving birth at that time. However, most are born with serious health complications.
During this trimester, many of the uncomfortable symptoms of pregnancy subside. Women may have more energy, increased appetite and higher sex drive for the first few weeks.
Some women may experience nasal congestion, tender gums and leg cramps. Backaches are common, as is slight brain fog. Because of fluid retention, fingers may feel tingly. Women also gain weight regularly until the baby is born.
Many women are pleased to notice their skin and hair look healthier.
To avoid symptoms of heartburn, women can eat smaller, non-greasy meals and avoid lying down after eating.
Women may begin to feel the “false labor pains” referred to as Braxton Hicks contractions. Typically, these start around week six, but women don’t feel them until the second or third trimester.
This is the body’s way of preparing for true labor. Braxton Hicks contractions feel like a mild menstrual cramp or abdominal tightening that comes and goes. This is a normal part or pregnancy and is nothing to worry about.
Unlike real contractions, Braxton Hicks contractions are mild, occur in the front of the abdomen or one specific area, and last from 30 seconds to two minutes. They are also inconsistent and sometimes subside when the woman moves or changes positions.
Real contraction pain starts in the back and wraps around the abdomen. It also becomes stronger with movement or position change and gets more intense with time.
- Doctors may use a needle to retrieve a sample of amniotic fluid from the womb between weeks 15 and 20 to test for substances that could lead to future complications.
- Additional tests are often performed between weeks 16 and 18 to look for potential abnormalities or birth defects.
- An ultrasound or sonogram is usually performed between weeks 18 and 20 to verify the expected delivery date and the baby’s anatomy, to record heartbeats and breathing movements, to check for additional fetuses and to identify potential abnormalities.
- If a diabetes test was not performed during the first trimester, women typically undergo the test between weeks 24 and 28 of their pregnancy.
Third Trimester
The third trimester lasts from week 29 to week 40, or until birth.
Around the 32nd week, the fetus’s eyes can open and close and the bones are almost fully formed. An infant born before the 37th week (preterm) is at an increased risk for developmental, hearing and visual problems.
Infants born during the 37th and 38th (early term) weeks face less serious health risks, but are usually not as healthy as babies born in the 39th and 40th weeks (full term). Babies born during the 41st week (late term) and after 42 weeks (post term) are also at a higher risk for complications.
During this trimester, women may feel more tired and develop hemorrhoids. The body experiences more aches and pains. Stretchmarks may appear because of swelling and stretching of skin. Breasts will leak as they prepare for breastfeeding. If women have sex, they may have spotting after.
If Braxton Hicks contractions didn’t start in the second trimester, they will begin around week 29. Women can sleep through one of these weak, false labor pains. If changing positions doesn’t make them go away, they will eventually go away on their own.
True labor contractions last between 30 and 90 seconds and increase in duration, coming closer together, as it gets closer to delivery time.
Prenatal Care
Almost a third of women who become pregnant experience some kind of complication. Prenatal care helps prevent the risk of pregnancy complications and increase a doctor’s chance of detecting complications if they occur.
Prenatal care refers to the healthcare women receive while pregnant. It includes checkups, screenings, and dietary and lifestyle changes. In a perfect world, women would begin prenatal care before they become pregnant. When that is not possible, women should begin prenatal care as soon as they realize they are pregnant.
- Obstetricians
- doctors who concentrate in pregnancy and childbirth
- OB/GYNs
- Obstetricians/gynecologists are doctors who concentrate in pregnancy and childbirth, in addition to women's health care
- Family practitioners
- doctors who offer a variety of services to people of all ages, usually a pregnant woman’s general practitioner
- Midwives
- may be licensed, professional midwives or certified nurses that concentrate in women’s healthcare, pregnancies and childbirth
Prenatal Supplements & Medication
A prenatal checkup before pregnancy involves testing for any diseases or conditions that could affect a pregnancy. Most women decide to either change or discontinue medications or potentially unhealthy habits during this visit. They may also begin taking prenatal vitamins, folic acid, calcium or iron supplements.
- Folic Acid
- helps prevent neural tube defects which affect the development of the spine and nervous system
- Calcium
- helps the fetus develop strong bones, nerves and muscles
- Iron
- helps carry oxygen to blood cells
- Prenatal vitamins
- usually contain adequate balances of folic acid, calcium and iron but lower doses of other vitamins and minerals that could be harmful
Weight Gain & General Health
Weight gain is a typical and healthy aspect of pregnancy. Most women should gain 25-35 pounds during pregnancy, but overweight women should only gain 15-25 pounds and underweight women should gain 28-40 pounds.
Although many women worry about gaining weight, a failure to do so could result in inadequate fetal growth or premature labor. Accordingly, most women should not start a weight-loss diet during pregnancy. Rather, they should begin a healthy diet if they do not already practice one.
Women should avoid foods that could contribute to foodborne illnesses, like unpasteurized cheese, milk or juice and raw meats including fish, eggs and deli meats. Additionally, some seafood contains high amounts of mercury which may harm the fetus.
- Don't smoke
- Don’t drink alcohol
- Don’t abuse drugs
- Get plenty of rest
- Eat a healthy diet
- Perform low-impact exercises
Pregnancy Diet and Exercise
For most women, eating an additional 500 calories a day is enough to properly nourish themselves and their babies, according to Cleveland Clinic. About 200 to 300 of these calories should come from whole foods with a lot of nutrients, such as whole grains, vegetables, fruits, leas meats and low-fat dairy.
- Get at least 1,000 milligrams of calcium a day from four servings of dairy or foods such as leafy greens, fortified cereals and bread, sesame seeds and almonds.
- Folic acid is especially important during pregnancy. Get at least 400 micrograms from fortified breads, rice, flour, cereal and pasta. Eat foods rich in folic acid, such as leafy greens, beans, citrus fruits, lentils and nuts.
- Women should get a total of 27 mg of iron a day from prenatal vitamins and foods such as leafy greens, beans, sardines, beef, pork and whole grains.
- Eat leafy greens, deep yellow or orange vegetables, milk and liver to get 770 mcg of vitamin A daily.
- Women need 600 international units of vitamin D a day from fortified milk or fatty fish, such salmon.
- Pregnant women should get at least 200 mg of DHA in prenatal vitamins or supplements.
- Eating two to three 4-ounce servings of safe fish a week is acceptable. For more information on safe fish, check the FDA’s Advice About Eating Fish.
- Limit caffeine to two 5-ounce servings of coffee, two 12-ounce servings of soda or three 5-ounce servings of tea.
- Avoid alcohol.
- Avoid overly salty foods, which could lead to water retention and elevated blood pressure.
Women should avoid foods that could contribute to foodborne illnesses, such as unpasteurized cheese, milk or juice and raw meats including fish, eggs and deli meats.
Women with healthy, normal pregnancies should exercise to maintain optimal health. But it’s important to discuss exercise routines with a health care provider first. Walking, swimming, stationary bicycling, modified yoga or pilates are good choices.
Dangerous Drugs During Pregnancy
Some avoidance of drug use during pregnancy is easily understood, such as the use of street drugs (illegal or illicit drugs) including cocaine, ecstasy and methamphetamines, heroin and marijuana. While about 1 in 20 women take street drugs during pregnancy, it is typically known that these substances are harmful to adults, so naturally they would also be harmful to a developing fetus.
But the safety of prescription drugs or even over-the-counter drugs and supplements during pregnancy may not be as well-known.
- Problems with the placenta
- Birth defects
- Withdrawal symptoms in the infant after birth
- Underweight babies
- Preterm labor (labor occurring prior to 37 weeks)
- Miscarriage (loss of pregnancy prior to 20 weeks)
- Stillbirth (when the baby dies in the mother’s uterus after 20 weeks)
The Centers for Disease Control and Prevention states that little is known about the effects of taking most medications during pregnancy. This is because, ethically, pregnant women are often not included in premarket studies to determine the safety and efficacy of a new drug or treatment. The CDC estimates that less than 10 percent of FDA-approved medications since 1980 have enough information to determine their real risk for birth defects.
However, it is necessary for some women to take medications during their pregnancy to treat certain health conditions, such as asthma, epilepsy (seizures), high blood pressure or depression. If the pregnant mother does not continue medication for the management of these and other health conditions, it can actually be more harmful to her health as well as the health of the unborn baby. It is always important for a pregnant woman to speak with her doctor before discontinuing medications.
OTC Drug Use in Pregnancy
According to an article published by American Academy of Family Physicians (AAFP), “despite the absence of randomized clinical trials to guide their use during pregnancy,” more than 90 percent of pregnant women take a prescription or over-the-counter (OTC) medication. Most OTC medications used during pregnancy are for allergy, respiratory, gastrointestinal or skin conditions. But acetaminophen, a pain reliever, is also used by approximately 65 percent of expecting mothers, although it’s generally considered safe to do so.
Cold medicines are also generally considered safe if taken short-term and outside of the first trimester. But AAFP advises pregnant women to use pseudoephedrine, a decongestant, with caution. Overall, doctors should be cautious in recommending, and mothers should be cautious in taking, any OTC medication during pregnancy due to the potential for adverse effects to occur to the developing fetus.
At least 10 percent of birth defects are believed to result from drug exposure via the mother, according to AAFP; and of all the new OTC drugs marketed between 1975 and 1994, 30 percent were previously prescription medications.
Alcohol Use and Smoking
The National Institutes of Health (NIH) recommends that pregnant women do not smoke, as this exposes the unborn infant to nicotine, carbon monoxide, and other harmful substances. Furthermore, smoking can keep the developing fetus from getting the nourishment they need and increases a mother’s risk of stillbirth or premature labor.
Because e-cigarettes are marketed as a safer alternative to smoking, some pregnant women may think it’s safe to vape while pregnant. But even if e-cigarettes have fewer toxic chemicals than cigarettes, they have been linked to serious side effects. Those that contain nicotine are especially harmful to developing babies and pregnant women. Nicotine can damage a developing baby’s brain and lungs, and flavored e-liquids may also be harmful to fetuses, according to the CDC.
The agency recommends quitting all tobacco products if you’re pregnant.
The NIH also warns against drinking alcohol during pregnancy, noting that “there is no known safe amount of alcohol a woman can drink while pregnant.” The NIH stated that drinking alcohol while pregnant can cause chronic physical and behavioral problems in children, including fetal alcohol syndrome, which is a condition that can result in facial abnormalities (including wide-set and narrow eyes), growth problems and nervous system problems.
Prescription Drug Interactions in Pregnancy
Adverse drug interactions may occur in pregnancy when certain drugs present potential harmful effects to the unborn baby and in some instances, the mother as well. These interactions can include increasing or reducing the overall effectiveness of a drug due to the woman’s pregnant state, or causing unexpected side effects to the mom or her baby.
Before taking any medications during pregnancy, and sometimes before pregnancy while planning to get pregnant or after pregnancy if breastfeeding, a woman should consult with her doctor about the known (and unknown) risks versus benefits to herself as well as her baby.
- Can I take this drug while pregnant?
- Can I take this drug with other drugs?
- Should certain foods, beverages, other products or activities be avoided while taking the drug?
- What are some possible signs of a drug interaction to look out for?
- How will the drug work in pregnancy? How might it affect the fetus?
- Is there more information available about the drug, the condition being treated and possible interactions during pregnancy?
Some examples of medications that have known interactions in the health of pregnant women and developing fetuses, include:
- Used to Treat
- Acne
- Harm to Mother
- Significantly increased risk of miscarriage and premature delivery
- Harm to Fetus
- High risk of birth defects, including intellectual disabilities, brain malformations, heart defects and facial abnormalities. Significantly increased risk of infant death.
- Used to Treat
- Depression, anxiety, OCD, panic attacks, PTSD
- Harm to Mother
- Depression during pregnancy can lead to postpartum depression, which is a serious condition requiring treatment. The benefits of treating depression during pregnancy sometimes outweigh the risks.
- Harm to Fetus
- Can cause birth defects, such as persistent pulmonary hypertension (in a newborn, this is defined as the failure of normal circulatory transition after birth), heart defects, respiratory distress, cleft palate, malformation of the skull and autism.
- Used to Treat
- High blood pressure
- Harm to Mother
- High blood pressure before and during pregnancy can increase a pregnant woman’s risk for preeclampsia and eclampsia.
- Harm to Fetus
- Black box warning: Fetal toxicity; Can result in fetal injury or death.
- Used to Treat
- High cholesterol; to reduce the risk of heart attack and stroke
- Harm to Mother
- Women should not breastfeed while taking rosuvastatin.
- Harm to Fetus
- Low birth weights, bone malformations and death in lab rats.
- Used to Treat
- Epilepsy (seizures), bipolar disorder, and migraine headaches
- Harm to Mother
- Risk for development of polycystic ovarian syndrome (PCOS) – health problem that affects a woman’s hormone levels, periods, ovulation, fertility and pregnancy
- Harm to Fetus
- Maternal exposure, especially during the first trimester, can increase the risk for serious birth defects affecting the brain, heart and limbs, including spina bifida (involving the spinal cord and backbone), cleft palate, penis abnormality, an extra digit on the hand and premature fusion of the skull
- Used to Treat
- Excessive sleepiness associated with narcolepsy, obstructive sleep apnea and shift work disorder
- Harm to Mother
- May be habit forming; may cause rare allergic reactions, worsening of psychiatric symptoms, and increases in blood pressure and heart rate
- Harm to Fetus
- Risk of birth defects, including congenital heart defects, orofacial clefts and hypospadias (a genital abnormality in boys)
- Used to Treat
- Nausea and vomiting during pregnancy
- Harm to Mother
- Ondansetron should not be used as a first-line treatment for symptoms of “morning sickness” in pregnancy. In addition, it should be avoided in the first trimester.
- Harm to Fetus
- Fetal heart malformation and increased risk of birth defects, including cleft palate
Common Complications
Even when women receive proper prenatal care and avoid dangerous drugs, they could still experience complications during pregnancy. This includes women who led healthy lives and maintained healthy weight before pregnancy. When a woman has health complications while pregnant, her pregnancy is considered high-risk.
High-Risk Pregnancies
A high-risk pregnancy can threaten the mother or the fetus’s life. With proper prenatal care, healthcare providers can detect and treat complications early to improve the chances of a healthy pregnancy.
- Health conditions
- like high blood pressure, diabetes or HIV
- Weight
- being underweight, overweight or obese
- Multiple fetuses
- teens and women older than 35
- Young or old age
- teens and women older than 35
High Blood Pressure
Hypertension (high blood pressure) occurs when arteries from the heart to organs narrow causing extra pressure. This makes it hard for blood to travel to the placenta and provide nutrients and oxygen to the fetus.
Women with hypertension before pregnancy should monitor and attempt to control it. Some women develop high blood pressure, called gestational hypertension, during pregnancy. About four percent of women develop the condition, and it almost always goes away after childbirth.
Gestational Diabetes
Gestational diabetes is another condition that develops during some pregnancies. It occurs when changes in hormones during pregnancy prevent the body from making insulin or using insulin properly. When this happens, glucose (sugar) builds up in the blood causing high blood sugar.
About eight percent of pregnant women develop gestational diabetes. If untreated, it can cause heart disease, vision problems, kidney disease or preeclampsia.
Preeclampsia
Preeclampsia is one of the most common causes of maternal death and one of the most serious complications associated with child-bearing.
Preeclampsia causes high blood pressure and can be fatal during and following pregnancy. Most deaths from preeclampsia happen in the days, weeks or months after a woman gives birth.
It affects 200,000 expectant and new mothers in the U.S. every year. Preeclampsia accounts for about 8 percent of all pregnancy related deaths in the U.S.
But it is more dangerous for African-American women. Preeclampsia accounts for nearly 12 percent of pregnancy-related deaths for non-Hispanic black women.
- First time being pregnant
- Previous history of preeclampsia
- High blood pressure, diabetes, kidney disease or lupus
- Being African American
- Being 35 years or older
- Carrying two or more fetuses
- Obesity
Symptoms of Preeclampsia
Women suffering symptoms of preeclampsia should seek immediate medical attention. Some women may not experience any symptoms even though they have preeclampsia. Their health care provider should monitor them for any warning signs.
- Abdominal pain
- Anxiety
- Headache
- High blood pressure
- Hyperreflexia (overreactive reflexes)
- Lower back pain
- Nausea or vomiting
- Decreased urination
- Shortness of breath
- Shoulder pain
- Sudden weight gain
- Swelling
- Vision changes
Preeclampsia that occurs after a woman gives birth is often misdiagnosed. Its symptoms mimic conditions people associate with normal childbirth. These can include headaches, swelling and stomach pain or other stomach problems.
- Changes to vision
- Decreased urination
- Excess protein in the mother’s urine
- High blood pressure (140/90 or higher)
- Pain in the upper abdomen
- Severe Headaches
- Stomach problems or pain
- Swelling
Preeclampsia causes high blood pressure and can lead to premature delivery or a large infant, increasing the need for a cesarean section. Preeclampsia can also lead to protein in urine or edema – fluid buildup in body tissues causing swelling.
Pregnancy Loss
A miscarriage is a loss of pregnancy from natural causes before the 20th week. It occurs in an estimated 20 percent of pregnancies. Signs of a miscarriage include vaginal bleeding, cramping and fluid or tissue passing from the vagina. Bleeding does not mean that a miscarriage is happening, but women should contact their health care provider if bleeding occurs.
After the 20th week, a loss of pregnancy is referred to as a stillbirth. Doctors cannot determine the cause of stillbirths in about half of all cases, but factors that could contribute to stillbirths include infections, chromosomal abnormalities, inadequate fetal growth, placental issues and a mother’s health issues.
Depression
Depression involves feelings of sadness, anxiety or emptiness that interfere with daily activities. About 13 percent of pregnant women and new mothers suffer from depression. Symptoms of depression can be mild or severe, but doctors can treat almost all of them. Women suffering for more than two weeks should contact their doctor.
A family history of mental health problems, changes in brain chemistry that occur during pregnancy, stressful life events and hormones all contribute to depression during pregnancy.
- Sadness
- Restlessness
- Moodiness
- Hopelessness
Postpartum Depression
Postpartum depression occurs after childbirth. The rapid change in hormone levels after childbirth or a decrease in levels of thyroid hormones after childbirth may lead to postpartum depression. Other factors like exhaustion, feeling overwhelmed, doubts about capabilities of being a good mom and lack of free time can contribute to postpartum depression.
- Talk to their healthcare provider
- Sleep as much as possible
- Avoid trying to be a “perfect” mom
- Ask friends and family for help
- Talk to family and friends about feelings
- Attempt to find free time
- Join a support group
- Anemia
- Iron deficiency can cause a tired feeling, shortness of breath and pale skin.
- Hyperemesis gravidarum
- Although nausea and vomiting are normal during the early stages of pregnancy, some women experience severe, long-lasting symptoms. The cause is unknown, but hyperemesis gravidarum can cause weight loss, dehydration and faint feeling.
- Infections
- Washing hands and avoiding risky foods can prevent most infections.
- Urinary tract infections (UTI)
- Bacterial infections in the urinary tract can cause pain when urinating, fever and nausea.
How to Get Pregnant
The amount of time it take for a woman to get pregnant depends on factors such as age, overall health and genetics. Nearly 85 out of 100 women who want to get pregnant and have unprotected vaginal sex succeed within a year.
Women trying to get pregnant should pay attention to days when they ovulate and plan vaginal sex around those days. This also applies to women who are planning to use insemination to get pregnant.
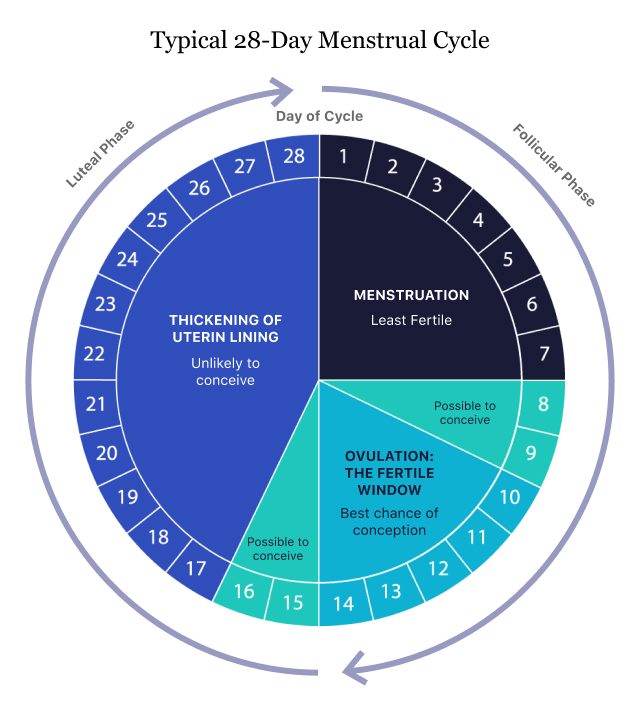
According to Planned Parenthood, ovulation usually starts about 14 days before your period starts. Five days before ovulation and the day of ovulation are the most fertile days. Sperm can live in the body for six days, and the egg survives for one day after it is released.
There are apps that make it easy to track the menstrual cycle. Most pharmacies and drugstores also sell ovulation predictor kits.
People trying to get pregnant should ask their health care providers for advice. Planned Parenthood also provides tips for getting pregnant and having a healthy pregnancy.
How Birth Control Affects Fertility
Most women in the U.S. use some type of birth control. In most cases, women who want children can stop their birth control. But, some forms of contraception may affect a woman’s ability to become pregnant.
Birth Control Pill
Most women choose a form of oral contraception, also known as “the pill.” More women are choosing to have babies later in life. This means many have been on the pill for several years to prevent pregnancy. The good news is fertility returns as soon as a few days after stopping the pill.
Birth Control Shot
Some women receive birth control shots such as Depo-Provera once every three months to prevent pregnancy. After three months, it is no longer reliable as birth control. But, because it goes into the muscle its effects linger. For some women, it can take about 10 months after the last shot for fertility to return.
Mirena and Other IUDs
An IUD is a small plastic implant inserted into the uterus. Most release hormones (Mirena) and one (Paragard) uses copper to prevent pregnancy.
One study showed long-term users of IUDs had a more difficult time getting pregnant than those who used the pill. Another showed a reduction in fertility in African American women.
IUDs may also increase the risk of pelvic inflammatory disease, which leads to infertility.
Labor
Labor is the process of childbirth in which the fetus and placenta leave the uterus.
During the final weeks of pregnancy, the fetus is still developing its lungs and brain. Thus, a woman should be pregnant for at least 39 weeks before giving birth to ensure the highest chance of a healthy outcome. However, a health care provider might recommend inducing labor sooner if there is a health risk to the fetus or mother.
Health care providers may use various devices to monitor the baby’s heartbeat during labor and the strength of contractions. They may use a special stethoscope belt wrapped around the abdomen called a Doppler transducer to monitor the baby. Electronic fetal monitoring uses a belt wrapped around the abdomen or electrodes placed on the part of the fetus that is closest to the cervix, usually the scalp.
Women can give birth in a number of different ways. The two general delivery methods include vaginal birth and cesarean sections, or C-sections.
Drugs that Induce Labor
If labor hasn’t started when it should, health care providers may use drugs to induce labor. Two drugs used to induce labor are Pitocin (oxytocin) and Cytotec (misoprostol).
Pitocin is a synthetic form of the hormone that causes contractions. Doctors administer it intravenously to start or strengthen contractions. Doctors will monitor the mother and baby and adjust the dose as needed. Labor usually starts 30 minutes after the drug is administered.
Side effects of Pitocin to the mother include: allergic reaction, nausea, vomiting, pelvic hematoma, heart rhythm irregularities, postpartum hemorrhage and death.
Side effects to the baby include: brain or nervous system damage, heart beat problems and fetal death.
Cytotec is not approved for inducing labor, but some doctors use it off-label. The FDA warns that using the drug can result in a torn uterus and severe bleeding. This may lead to a hysterectomy or death of the mother or baby. The risk of side effects is greater in women who have had previous uterine surgery, several previous births or a previous C-section.
- The woman feels relief or lighter, because the fetus moves from the rib cage to the pelvic area (lightening)
- The woman notices clear, pink or slightly bloody discharge called show as the cervix begins to dilate
- Contractions begin
- Vaginal discharge changes color
- Pelvic pressure occurs
- Lower backache occurs
- Abdominal cramps occur
- Less fetal movement
- Water breaking (when the amniotic sac ruptures)
- Diarrhea
- Nesting (preparing for the baby)
-
First Stage
During the first stage, the woman’s body is working to fully open her cervix and prepare for delivery. It is the longest stage of labor, typically lasting about 12 to 19 hours. A doctor will monitor the mother’s progress by periodically checking her cervix. Towards the end of this first stage of labor, contractions will become longer, stronger and closer together. Positioning and relaxation techniques can assist women in staying somewhat comfortable throughout this time. Some women may opt for medication, such as an epidural, which is a type of anesthesia administered via a shot in or around the spine that numbs part of the body to block pain. Sometimes a woman’s doctor may have to manually rupture the membranes (amniotic sac) in order to speed along a birthing process that is progressing too slowly, although some studies have shown that this is not particularly helpful in shortening the length of labor. The transition is the most difficult phase of stage one as the contractions become stronger with little time to relax in between. Women can experience nausea and feel shaky during the transition. When the cervix reaches 10 centimeters, it is fully dilated and stage one comes to an end.
-
“Active” Stage
The second stage involves pushing and the delivery of the baby. This stage can last anywhere from 20 minutes to two hours. Pushing occurs during contractions with the mother resting in between. A woman can give birth in various positions including squatting, sitting, kneeling or lying on her back. When the baby’s head is completely visible it is called crowning. A doctor may perform an episiotomy, which involves making a small cut to enlarge the vaginal opening and avoid unintentional tearing, to assist in delivery. Various tools, such as forceps or suction, can be used to help guide the baby through the birth canal. This is called an assisted vaginal delivery. After the baby is born, the umbilical cord is cut.
-
“Placental” Stage
After the delivery of the baby, the mother must then deliver the placenta, also referred to as the afterbirth. This is the shortest stage of labor lasting only five to 30 minutes. Contractions occurring after the birth of the baby signal when it’s time to deliver the placenta. This normally takes place about five to 30 minutes following the delivery of the newborn. A woman might experience chills and shakiness during this stage. After the placenta is delivered, labor is over, and the doctor will repair any cuts or tears.
Medicated Birth
A “medicated” birth is the most popular delivery method in the U.S. About 61 percent of women give birth while receiving pain medication, usually in the form of an epidural block, spinal block or general anesthesia. An epidural is injected into the spine, and a spinal block is injected into the spinal fluid. If given anesthesia, the woman is asleep during the delivery.
Although non-medicated births are growing in popularity, there is no evidence that delivering a baby while medicated affects the baby’s Apgar score – a test that measures a baby’s health immediately after it is born – or increases the chance of a C-section.
Unmedicated Birth
About 39 percent of U.S. women give birth using no pain medication. Instead, they may rely on relaxation and breathing techniques to reduce pain. Many women feel a sense of empowerment by giving birth without the assistance of medication.
Some women avoid medication, because it may cause their blood pressure to drop, affect the speed of labor or cause them to become nauseated.
Cesarean Section
A C-section is a surgical procedure in which a doctor makes an incision in the mother’s abdomen and uterus to deliver the baby through. After the delivery, the doctor closes the uterus with stitches that eventually dissolve and the abdomen with staples or stitches. About 33 percent of babies are born via C-section.
C-sections are generally considered safe, but like all surgeries, complications can occur. Recovery usually takes longer, infants may be more likely to experience breathing problems and future pregnancies could be affected. Women who have had a past C-section give successful vaginal births about 75 percent of the time.
- A woman is carrying multiple fetuses.
- The fetus is too large.
- The fetus is positioned feet first instead of head first (breach).
- The mother has a disease or infection that could be transmitted to the fetus, such as HIV or herpes.
- There are problems with the placenta.
- Complications in labor involving the mother occur, such as the cervix failing to dilate properly.
- Complications in labor involving the fetus occur, such as problems with the umbilical cord or an abnormal heart rate.
Alternative Birthing Methods
Alternative methods to medicated births (using epidurals and other anesthetics or pain relievers), such as immersion in water, hypnobirthing (using hypnosis), and utilizing doulas and birthing coaches that focus exclusively on the mother throughout the labor and delivery process, and even for a short time after birth (postpartum), are drawing increased interest among pregnant women, U.S. News & World Report said.
Doulas Versus Midwives
DONA International defines a doula as a trained professional “who provides continuous physical, emotional and informational support to a mother before, during and shortly after childbirth to help her achieve the healthiest, most satisfying [childbirth] experience possible.”
Doulas receive training to support mothers and families emotionally and physically, but they are nonclinical professionals, according to Jessica Costa, a certified nurse midwife with Cleveland Clinic.
This means they can coach women during labor with relaxation, pushing and breathing, but they do not deliver the baby. They provide emotional support during pregnancy and during the postpartum period, but they cannot give medical advice.
In contrast, there are different types of midwives with varying levels of education and experience. Each state has its own laws governing what midwives can and cannot do.
Nurse Midwives, Certified Nurse-Midwife (CNM)
Nurse midwives are trained in midwifery and nursing. They are registered nurses with master’s degrees who can deal with low-risk pregnancies and deliver babies in hospitals or at a mother’s home. They can also perform gynecological exams and advise on matters of women’s health.
Many hospitals have CNMs on staff. They have passed a national exam and can practice in all 50 states and the District of Columbia.
Direct-Entry Midwives
Certified Midwives (CM) and Certified Professional Midwives (CPM) are called direct-entry midwives. They don’t have nursing degrees, but CMs have master’s degrees in health and are trained and certified in midwifery. Only a handful of states recognize CMs and allow them to legally practice.
CPMs must demonstrate knowledge and experience in providing midwifery services out of hospital settings and must have graduated from an accredited midwifery education program. Twenty-seven states recognize CPMs.
The Bradley Method
The Bradley Method is a birthing technique taught in a 12-week class that takes place throughout the last trimester of pregnancy. This method was developed by Dr. Robert Bradley in the late 1940s and it encourages women to deliver naturally, with little or no drug intervention, in the presence of their partners, looking to them as a coach.
The courses focus on nutrition, exercise, relaxation and pain management, and teach women how to “tune into their bodies” and find positions effective in easing labor pains and preparing for each stage of labor. This method is supposed to be successful in assisting women with their birthing plans and avoiding surgical deliveries (C-section).
HypnoBirthing
Hypnobirthing is a labor pain relief program developed by Marie Mongan in 1989. It focuses on eliminating a woman’s birthing fears with self-hypnosis as well as breathing and relaxation techniques.
According to the American Pregnancy Association, women who have used this method report “feeling lost in a daydream, relaxed, calm, aware and in control.”
HypnoBirthing involves courses with an instructor, along with self-hypnosis exercises that can be used at home. Mongan created the program referencing the natural birth theories of Drs. Grantly Dick-Read and Jonathan Dye.
Lamaze
Lamaze is a birthing technique that involved the proper use of breathing. Women are taught to control their breathing, change positions and walk throughout labor. Dr. Ferdinand Lamaze developed the method that emphasizes distraction during contractions “decrease the perception of pain and reduce discomfort,” according to the American Pregnancy Association.
This method also encourages the support and participation of the mother’s partner, with classes focusing on partner involvement in controlled deep breathing techniques, massage, concentration and learning how to maintain control during labor.
Even though Lamaze is considered a natural birthing method, women using this method can still opt for an epidural if they should decide it’s needed.
Water Delivery
Some women may find that giving birth in a warm tub of water is relaxing, and the buoyancy is believed to help relieve discomfort and pressure. Some also believe that the water “helps the baby enter the world with less light, sound and dramatic change,” as stated by the American Pregnancy Association. However, U.S. News & World Report interviewed the chief of maternal-fetal medicine and director of obstetrics at University of Florida Health, Anthony Gregg, who concluded “there’s no evidence that [a water delivery] improves perinatal outcomes, or decreases the C-section rate.” He did, however, state that it is helpful in decreasing pain, reducing the need for anesthesia and shortening delivery times.
But OB-GYN at Cleveland Clinic’s Hillcrest Hospital in Ohio, Monica Svets, said that water births have not been studied enough to be recommended, and the American Pregnancy Association warned that this method is definitely not recommended for women with high-risk pregnancies, and that deliveries should occur out of water in situations where complications arise.
Non-Recumbent Birthing Positions
A woman can give birth in a number of different positions. The supine recumbent position is the traditional position for giving birth in most healthcare facilities, because many of the medical devices and monitoring tools used in hospitals limit other options.
However, women squat while giving birth in many parts of the world, including Asia, Africa and parts of South America. There is not a perfect position to give birth in, but some experts recommend changing positions during labor to help with pain.
- Rocking
- Standing
- Lunging
- Kneeling
- Squatting
- Leaning forward while sitting
- Extending legs while sitting
- Lying on the side
- Reflexology
- Reflexology is one of the most popular non-medicinal methods of pain relief for delivery, and it can be used in almost any delivery method. It focuses on flexing certain areas of the body, including the hands, feet and various muscles. There are a variety of scientific theories that support the idea that reflexology may help relieve pain.
- Acupuncture and Acupressure
- Acupuncture involves inserting very fine needles into the skin and rotating, heating or electrically stimulating them to relieve discomfort. Acupressure involves applying pressure to similar points on the body to relieve discomfort. Both are used to relieve discomfort during labor, primarily in Asian cultures.
- Herbs
- Herbal treatments usually involve a variety of ingredients including roots, leaves, barks, twigs, fruits, berries and flowers. Some people take specific herbal supplements concocted to boost a woman’s strength and energy during labor. Other herbal treatments are used as washes or cleanses.
- Aromatherapy
- Aromatherapy uses scents and smells to boost a woman’s mood during labor. Many women use aromatherapy during labor, but there are no studies that prove its effectiveness.
Breastfeeding
Breastfeeding is the most popular way to feed and nourish an infant. Breastfeeding should begin within one hour after birth, and can occur up to 12 times per day in the first weeks of life.
Many infants are breastfed exclusively, receiving no other form of nutrition for the first six months of their lives.
Whether or not a woman chooses to breastfeed is a personal decision every new mother has to make for herself and her baby. However, the U.S. Department of Health and Human Services (HHS) does list several benefits for not only the newborn, but the mother as well.
Benefits of Breastfeeding
A mother’s first milk is called colostrum, and it’s referred to as “liquid gold” due to its deep yellow color. This thick type of milk is made during pregnancy and just after birth, and it is extremely rich in nutrients and antibodies that protect your newborn from infections.
Colostrum also helps a new infant’s digestive system to grow and function. As a baby grows, its mother’s milk changes, becoming mature milk within three to five days after birth. This milk consists of sufficient amounts of fat, sugar, water and protein. It is thinner than colostrum, but still packed with nutrients and antibodies.
- Asthma
- Childhood leukemia
- Childhood obesity
- Ear infections
- Eczema
- Type 2 diabetes
- Diarrhea and vomiting
- Lower respiratory infections
- Disease that affects the gastrointestinal tract in premature babies
- Sudden infant death syndrome (SIDS)
Although not quite as lengthy of a list, the mother is not without her own equally important benefits. Breastfeeding not only helps a mother to heal following childbirth, but leads to a lower risk of Type 2 diabetes, certain types of breast cancer and ovarian cancer. As a bonus, breastfeeding may help women lose weight. HHS states that “many women who breastfed their babies said it helped them get back to their pre-pregnancy weight more quickly,” however, experts are still researching the link between breastfeeding and weight loss.
But most importantly, HHS finds that breastfeeding can save lives. The governmental health department said research shows that if 90 percent of mothers breastfed their infants exclusively in their first six months of life, nearly 1,000 deaths among infants could be prevented each year. Additionally, breastfeeding is more cost-effective, more convenient, and keeps mom and baby close.
When Is Breastfeeding Not Beneficial?
Breastfeeding isn’t always the more beneficial choice. The Centers for Disease Control and Prevention (CDC) pointed out that in rare instances, human milk is not recommended for newborns.
These exceptional circumstances include when an infant is diagnosed with galactosemia (a rare genetic metabolic disorder that affects a person’s ability to metabolize — process — the sugar galactose present in many foods), and when the mother has certain infectious diseases, such as the human immunodeficiency virus (HIV) or tuberculosis, is using or dependent upon illegal drugs, or is taking prescribed cancer chemotherapy treatments or undergoing radiation therapies.
Breastfeeding Complications
New mothers should expect to have some discomfort, breast fullness or nipple tenderness as they begin breastfeeding their infant, especially if it is their first time nursing or they are first-time mothers. Although rare, it is also sometimes possible that a mother will produce too little milk. Frequent feedings, adequate rest, good nutrition and staying hydrated are all ways in which a mother can maintain a good milk supply.
- Alternating nursing positions to keep milk ducts emptying regularly
- Allowing nipples to air dry after each feeding
- Avoiding excessive use of soap on the breast and nipples
- Wearing cotton bras and keeping breast pads as clean and dry as possible
- Using lanolin on the nipples after feedings
Complications of breastfeeding can include:
Engorgement
When the milk ducts do not adequately empty during feedings, the breasts can become hard, painful, hot, and taut or shiny in appearance. Once the breasts are engorged, feeding can become painful and difficult, further exacerbating the problem.
Thrush
Thrush is a common yeast infection that can be passed from the mother to the infant, or from the infant to the mother, during breastfeeding. This type of yeast infection (Candida albicans) thrives in warm, moist areas, which make the baby’s mouth and the mother’s nipples prime locations for its growth.
Symptoms of thrush in the mother may include deep-pink nipples that are tender and uncomfortable, especially during feedings. The infant may have white patches and increased redness in the mouth, diaper rash or a change in mood.
Antifungal medications can help to clear the infection.
Plugged Duct
Tender spots or lumps in the breast are indicative of plugged milk ducts. When milk ducts become plugged, the milk is unable to be expressed freely. This condition can be uncomfortable or even painful, but it typically does not lead to more severe symptoms, such as fever, when treated properly with rest, moist heat, massage and pumping often in between feedings to completely empty the breast.
Mastitis
Mastitis is a breast infection and one of the more serious complications of breastfeeding. When a plugged duct or cracked nipple goes untreated, it can result in mastitis. This serious condition can also be caused by anemia, stress or fatigue.
- High fever
- Flu-like muscle aches
- Fatigue
- Headache
- Intense, localized pain
- Red, hot and swollen breast
Antibiotics may be a necessary part of treatment. It is important to note, however, that the use of antibiotics can sometimes lead to thrush. Additionally, some medications, including antibiotics, may be passed from the mother to the infant via breast milk.
Reminder:
Pregnancy can be a rewarding experience, culminating in bringing a new life into the world. Women must be open with their health care provider to identify and address health issues throughout pregnancy.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

